Manifestations of syphilis on the hands. Skin manifestations of syphilis - photo. Nasal lesions due to syphilis
“Behavioural disease”, “French disease”, “German disease”. The names of syphilis are varied, as are the symptoms. Modern trends are forcing society to become more literate in health and medicine. So…
What is syphilis
Syphilis is an infectious venereal disease with a wave-like course that affects all systems of the body.
The causative agent of syphilis is Treponema pallidum. The course of the disease occurs in several stages:
- The incubation period involves the spread of the pathogen through organs and tissues through the circulatory and lymphatic systems with further reproduction. This stage has no clinical manifestations. Lasts within one month;
- The period of primary syphilis begins with the appearance of characteristic skin changes at the site of penetration of the pathogen. As well as the involvement of regional lymph nodes in the process. Duration of the period is 1-2 months;
- secondary syphilis. The stage is long (up to several years) with an undulating course. Many body systems are already involved in the disease. Now periods of acute clinical manifestations will alternate with periods of imaginary well-being;
- tertiary syphilis. With modern medical capabilities, this is a rare occurrence. It manifests itself in the absence of treatment in the form of irreversible changes in organs. It ends in disability or death for the patient.

Skin syndrome in primary syphilis
One of the obligatory manifestations of pathology is skin syndrome. It is important not to confuse or substitute concepts! There is no separately existing disease “cutaneous syphilis”!
At different stages of the disease, the rash will have different characteristics and localization. Today real photos available for everyone to view and study.
In order not to be just scared, but to be armed, let's understand all the variety of manifestations of skin syphilis!
The end of the incubation period will be the first sign on the skin - chancre (also known as a syphilitic ulcer). At the same time, specific changes in blood tests are still silent!

According to localization, genital and extragenital chancre are distinguished. But this will certainly be the site of primary penetration of the pathogen (mucous and skin of the genital organs, anal area, skin of the thighs, bikini area, abdomen, mucous membranes of the lips, oral cavity, upper respiratory tract).
Externally, the chancre has the appearance of a rounded erosion, with smooth edges. It’s not for nothing that education is called solid. Indeed, chancre resembles cartilage to the touch.
Most often, a syphilitic ulcer is single, up to several centimeters in size. It does not cause any particular concern to the patient, other than the unaesthetic appearance. The surrounding tissues and lymph nodes are still intact.

Atypical types of chancre deserve special attention.
This is a chancre-felon, when the primary focus is localized on the first phalanx of the finger and copies the symptoms of felon. The course involves pronounced inflammatory manifestations.
This is chancre-amygdalitis, simulating unilateral tonsillitis, but without the pain and intoxication component.
This is indurative edema, when the affected area does not have clear boundaries, but looks like a widespread dense infiltrate.

Skin syndrome in secondary syphilis
The spread of various types of rash diffusely, including the palms and soles, signals the transition of the disease to the stage of secondary syphilis. Many syphilitic skin lesions have led to
The International Classification of Diseases, Tenth Revision, even provided a separate niche for this condition and included “Secondary syphilis of the skin and mucous membranes” as a separate unit.
Syphilis on the skin is now characterized by polymorphism (variety) of rashes: roseolous syphilide, papular syphilide, condylomas lata, syphilitic leucoderma, syphilitic tonsillitis, syphilitic alopecia. And now more details...

Roseola syphilide. The most common manifestation of secondary syphilis is on the skin. Occurs in 80% of patients. It looks like multiple pink spots up to 1.5 cm in diameter, which are scattered over the skin of the torso and limbs.
The spots do not rise above the skin, turn pale when pressed, do not peel or itch. Resolution of the rash occurs on average in 2-3 weeks, sometimes up to 6 weeks. But after a while the 2nd wave comes.
The rash is now larger, paler, and tends to coalesce. It should be noted that there are also rare types of roseola: follicular and scaly.

Papular syphilide. This type of rash appears both along with roseola and independently. Papules are nodules located subcutaneously.
Depending on the size, nodules are divided into types: millet-shaped, lenticular, coin-shaped, plaque-shaped. Papules are localized scattered throughout the body, often on the mucous membranes of the genital organs, oral cavity, pharynx, and larynx.
Most of the time there is no pain. With the exception of the rash located in the folds. There is a high probability of secondary infection and the transition of papules to weeping erosions.
Important! The liquid separated from the erosion contains a huge amount of pale treponema. Therefore, in such cases, it is advisable to remember the risk of contact and household infection.

Wide condylomas. The problem of condylomas formation occurs in 5-10% of patients. Representatives of the fair sex are mostly unlucky. The favorite location is the perineum, sometimes the skin of the inner thighs.
The process begins with the grouping of papular rashes in the above areas and the gradual formation of plaques. The plaques merge into large areas, a wide stalk is formed and continues to spread to nearby areas.
The surface of condylomas is covered with scales and plaque gray. The exudate released from the surface contains a huge number of pathogens, which makes the patient very contagious.
Without treatment, the uncontrolled growth of condylomas lata can spread the formations to the mammary glands and armpits.

Syphilitic leucoderma. The rash appears as patches of uneven skin pigmentation. The affected areas of darkening first appear, which then transform into large white spots.
The skin in the area of the shoulder girdle, back, lower back, abdomen, and rarely the extremities is affected. Doctors distinguish spotted and lacy forms of leukoderma. With spotty, isolated foci are in familiar places.
With a lace shape, the spots merge into intricate patterns. This fusion around the neck has received the romantic name “Venus necklace”.
Interestingly, Treponema pallidum is found in surface layers dermis only in areas with spotted leukoderma.

Syphilitic alopecia. There are two reasons that cause hair loss due to syphilis. This is either the lack of hair growth in places where scars form after the rash resolves. Or their loss as a result of the course of the disease and a decrease in the body’s defenses.
In any of the cases, a characteristic sign is the focality of the lesion, scattered areas of baldness throughout the head.
In this case, the scalp resembles moth-eaten fur. And hairless skin has no specific changes. Hair growth can be restored by choosing the right treatment.

Syphilitic sore throat. A condition that occurs if, during primary syphilis, chancre is localized on the mucous membrane of the pharynx and tonsils. Then the secondary stage of development will imitate the course of a sore throat.
Initially, with the coloration of the palate and tonsils in a bluish-red color. This is followed by the appearance of erosions (ulcers) and the spread of a gray rash over the entire surface of the oral cavity.
The process is accompanied by intoxication and hyperthermic syndrome, peripheral lymphadenitis.

Skin syndrome in tertiary syphilis
Rare, but still occurring, is tertiary syphilis. Occurs in untreated or undertreated patients. Tertiary syphilides are skin lesions in the form of tubercles or gummas.
They are represented by deep infiltrates in which the body has “immured” Treponema pallidum. Nodular syphilide looks like small (5-7 mm) subcutaneous nodules scattered in large numbers.
Whereas gummas are large nodes, often not numerous. Elements of the tertiary period with a malignant course.
At the site of destruction, they will form ulcers and scars, involving the underlying bone and cartilaginous structures in the process of destruction. In this case, there are no acute inflammatory phenomena.
You've probably seen photos of a saddle nose change. So this is it clear example irreversible destruction bone tissue with untreated syphilis.

Skin syndrome in congenital syphilis
I would like to dwell separately on the types of skin manifestations of congenital syphilis.
Congenital syphilis is a form of syphilis that occurs when the fetus is infected during fetal development.
Skin syndrome will be one of the clinical manifestations.
Papular eruptions. Papules are located in the perineal area, on the buttocks, palms and soles.
The mucous membranes of the oral cavity and nose are also involved. Characteristic is the radial arrangement of papules and scars after their resolution on the skin of the face, and especially around the lips.
Pemphigus of the skin. A condition characterized by blistering rashes. The favorite localization of the latter is on the palmar and plantar surfaces of the extremities.

Differential diagnosis of skin manifestations
As can be seen from the description of the skin syndrome, it is quite diverse. It is not for nothing that syphilis has been called “monkey disease” since ancient times, referring to the variety of its masks.
The clinical picture requires differential diagnosis with dermatological, gynecological, urological, dental and other diseases.
Let's look at some specific examples.
Hard chancroid is differentiated from psoriasis, lichen planus, balanoposthitis, scabies, and erosions caused by other STD pathogens.
With an extragenital location of the chancre, the latter can be regarded as a boil, carbuncle, tonsillitis, or stomatitis.

Often diagnostic errors are caused by secondary syphilis. The rashes are disguised as psoriasis, different types lichen, toxicoderma, epidermophytosis, syphilitic alopecia must be distinguished from other types of alopecia, trichophytosis.
Condylomas lata are differentiated from papillomavirus condylomas and hemorrhoids.
It is important for doctors of different specialties to remember the visual characteristics of many types of rashes to differentiate and establish the correct diagnosis. Here, specialists are helped by characteristic signs and photographs of real patients.
The best prevention of sexually transmitted diseases is the culture and literacy of intimate communication. Be healthy and loved!
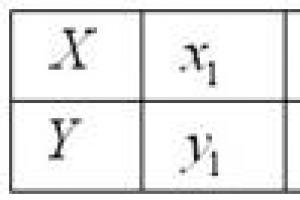
The manifestations of such a serious disease as syphilis can vary significantly at different stages. This allows the venereologist to accurately determine the disease itself, as well as the degree of its neglect. However, it should be borne in mind that sexually transmitted syphilis may change its clinical picture and symptoms in each specific case.
Therefore, knowledge of the general features and manifestations of the various stages of syphilis allows us to identify the disease in a timely manner and begin its treatment as early as possible, since over a long period of time it has a sharply negative effect on the internal organs and human health in general.
General manifestations of the disease
If we consider the general symptoms of syphilis, then it is necessary to take into account the current stage of the disease and the clinical picture as a whole. In the most general form, the symptoms of the current disease manifest themselves as follows:
- the appearance of a characteristic rash on the body;
- the appearance of a chancre that is hard to the touch;
- swollen lymph nodes;
- at the site of introduction of a pathogenic infection (treponema pallidum, which is the root cause of the disease);
- the formation of tubercles on the surface of the skin, which then begin to form on the mucous membrane of the internal organs.
The symptoms of syphilis are quite characteristic, therefore, with careful attention to one’s own health, it becomes possible to identify it at the earliest possible stage of development. Chancre can be considered the main manifestation of syphilis; its localization and size may vary. Depending on the degree of neglect of the pathology, the size of the chancre gradually increases, and the edges become ulcerated. This condition occurs in the later stages of syphilis development, and the treatment method must take into account both the prevalence of the pathology and the body’s susceptibility to the drugs used.
Elena Malysheva describes the general signs of syphilis in this video:
Skin manifestations of syphilis
With the course and gradual worsening of syphilis, various changes occur in the body that provoke deterioration general condition health and the manifestation of more and more new symptoms. The most pronounced changes are those that appear on the skin and can be diagnosed by visual examination by a dermatologist.
However, before starting treatment, it is necessary to clarify the preliminary diagnosis, which will allow you to avoid possible medical errors and create a treatment plan that will best restore the body and relieve the external manifestations of the disease. Diagnosis of syphilis is accompanied by taking a series of tests and examining the skin, which is more affected when the disease worsens.
Papular rash as one of the manifestations of syphilis on the skin (photo)
Rashes
At the early stage of development of the pathology, changes in the skin in the form are most often observed, which can be few in number, which complicates further diagnosis of the disease, or numerous. The rashes differ in their appearance, area of distribution and localization depending on the stage of the disease: at the initial stages they are less pronounced, and as the disease worsens they become more noticeable and voluminous.
Changes in skin rashes as syphilis worsens are as follows:
- initial stage characterized by the formation of hard chancre, which at first has a not very pronounced area, then becomes increasingly dense and its surface is eroded with the appearance of an ulcerative surface. At the site where the cause of the disease, Treponema pallidum, is introduced, an area of altered skin first appears, which transforms into and, as the pathology deepens into the body, becomes more noticeable and rises above the surface of the skin. The duration of the initial stage is about two months, during which an increase in the size of chancre is noted;
- at the second stage the rashes change. They acquire greater density, their surface becomes more glossy and eroded. The affected area increases, the size increases. In the absence of treatment at the second stage, the disease quickly transitions to the next, third stage, in which the prognosis becomes worse, and there is a high probability of many negative consequences for the patient’s health;
- third stage manifests itself in the form of a significant area of skin lesions, the rashes are repulsive in nature.
The manifestations of syphilis can vary, and the disease occurs in waves, with pronounced periods of exacerbation and remission. At the same time, there is an increase in the number of clinical manifestations, in which the patient’s general condition worsens, the degree of functioning of the immune system decreases, and the pathological pathogens of the disease that are destroyed under the attack of immune cells, when dying, release a poison dangerous to health.
This video will tell you more about the manifestations of the disease at different stages:
Skin spots
As syphilis progresses, areas of discoloration appear on the skin: having a pronounced bright pink color, they gradually, as the disease worsens, increase the affected area, and can cause and do change the appearance of the patient’s skin for the worse.
Which appear on the skin should be differentiated from other dermatological pathologies, which are accompanied by the appearance of spots on the skin with a modified color and surface condition. Such modified spots on the skin are called syphilitic; usually they are not inclined to unite, but their area gradually increases as the disease worsens. This condition worsens the appearance of the patient's skin.
The spots formed during syphilis are not prone to ulceration and are located chaotically. Such changes in the condition of the skin do not go deeper than the upper layer of the skin.
Ulcers
 Ulcerations of the skin surface are most often observed in more advanced areas of the skin, in the absence or insufficiency of treatment. Superficial ones gradually form at the location of the chancre, at the site of the root cause of the syphilitic infection. It is in this place that a compaction initially forms, which, in the absence or insufficiency of the therapeutic effect, increases in size, its surface changes its appearance.
Ulcerations of the skin surface are most often observed in more advanced areas of the skin, in the absence or insufficiency of treatment. Superficial ones gradually form at the location of the chancre, at the site of the root cause of the syphilitic infection. It is in this place that a compaction initially forms, which, in the absence or insufficiency of the therapeutic effect, increases in size, its surface changes its appearance.
Typically, ulcers on the surface of the skin occur as the disease develops and the pathological process worsens. Starting from the second stage of this disease, the skin begins to change, ulcerations appear at the site, which cause a lot of inconvenience to the patient and change the appearance of his skin for the worse.
Ulcers can also cause severe pain, since in these places the skin becomes more susceptible to any mechanical stress and is quickly injured.
This video will tell you how the disease manifests itself on the skin:
Secondary syphilis begins with the spread of pale treponema with blood throughout the body, which usually occurs 6 - 8 weeks after the appearance of chancre or 9 - 10 weeks after the primary infection. In some patients, syphilitic polyadenitis persists in the initial period. In 60% of cases, patients retain signs of primary syphiloma (hard chancre).
A massive release of bacteria into the bloodstream (syphilitic septicemia) is characterized by symptoms of intoxication - increased body temperature, severe headaches and muscle-joint pain, weakness, and general malaise. A rash appears on the skin and mucous membranes (secondary syphilides, secondary syphilomas), and internal organs, osteoarticular and nervous systems are involved in the pathological process. Periods of a pronounced clinical picture are replaced by a hidden, latent course. Each new relapse is characterized by fewer and fewer rashes. At the same time, the rash becomes larger and less intensely colored. At the end of the second stage of syphilis, monorelapses occur, when the clinical picture is limited to a single element. The well-being of patients suffers little. The duration of secondary syphilis is 2 - 5 years.
The rash with secondary syphilis usually resolves without a trace. Lesions of internal organs, musculoskeletal system and nervous system are mainly functional in nature. In most patients, classical serological reactions are positive.
The secondary period of syphilis is the most contagious. Secondary syphilides contain a huge amount of pale treponema.
Rice. 1. Symptoms of secondary syphilis - rash (papular syphilide).
Rash due to secondary syphilis
Secondary syphilis is characterized by the appearance of a rash on the skin and mucous membranes - secondary syphilides. The rash with secondary fresh syphilis is abundant and varied (polymorphic): spotted, papular, vesicular and pustular. The rash can appear on any part of the skin and mucous membranes.
- The most abundant rash at the first rash, often symmetrical, the elements of the rash are small in size, always brightly colored. Often against its background one can detect residual (chancroid), regional lymphadenitis and polyadenitis.
- Secondary recurrent syphilis is characterized by less profuse rashes. They are often grouped to form fancy patterns in the form of garlands, rings and arcs.
- The number of rashes in each subsequent relapse becomes less and less. At the end of the second stage of syphilis, monorelapses occur, when the clinical picture is limited to a single element.
Elements of the rash in secondary syphilis have some features: high prevalence at the beginning of the secondary period, sudden appearance, polymorphism, clear boundaries, peculiar coloring, lack of reaction of surrounding tissues, peripheral growth and subjective sensations, benign course (often the rash disappears spontaneously without scarring and atrophy), high contagiousness of the elements of the rash.


Rice. 2. Manifestations of secondary syphilis - syphilitic seizure.
Syphilitic roseola
Syphilitic roseola of the skin
Syphilitic roseola (spotted syphilide) is the most common form of damage to the mucous membranes and skin in early secondary syphilis. It accounts for up to 80% of all rashes. Syphilitic roseola is spots from 3 to 12 mm in diameter, from pink to dark red in color, oval or round in shape, do not rise above the surrounding tissues, there is no perifocal growth and peeling, the spots disappear with pressure, there is no pain and itching.
Roseola is caused by vascular disorders. In the dilated vessels, over time, the breakdown of red blood cells occurs with the subsequent formation of hemosiderin, which causes the yellowish-brown color of old spots. Roseolas that rise above the skin level often peel off.
The main locations for roseola are the trunk, chest, limbs, abdomen (often the palms and soles) and sometimes the forehead. Roseola are often located on the mucous membrane of the oral cavity, rarely on the genitals, where they are hardly noticeable.
Elevated, papular, exudative, follicular, confluent - the main forms of spotted syphilide. With relapses of the disease, the rash is more sparse, less colored, and tends to group with the formation of arcs and rings.
Spotted syphilide should be distinguished from pubic lice bites, pink lice, infectious roseola, measles, rubella and marbled skin.


Rice. 2. Rash due to secondary syphilis - syphilitic roseola.

Rice. 3. Signs of secondary syphilis - syphilitic roseola on the skin of the torso.
Syphilitic roseola of the mucous membranes
Syphilitic roseola in the oral cavity is located isolated, sometimes the spots merge, forming continuous areas of hyperemia in the tonsils (syphilitic tonsillitis) or soft palate. The spots are red, often with a bluish tint, sharply demarcated from the surrounding tissue. The general condition of the patient rarely suffers.
When localized on the mucous membrane of the nasal passages, dryness is noted, and crusts sometimes appear on the surface. On the genitals, syphilitic roseola is rare and always inconspicuous.


Rice. 4. Syphilitic roseola in the oral cavity - erythematous sore throat.
Syphilitic roseola is a typical manifestation of early secondary syphilis.
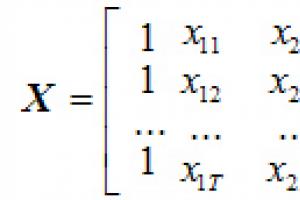
Papular syphilide
Papular syphilide is a dermal papule that is formed as a result of an accumulation of cells (cellular infiltrate) located under the epidermis in the upper dermis. The elements of the rash have a round shape, are always clearly demarcated from the surrounding tissues, and have a dense consistency. Their main locations are the trunk, limbs, face, scalp, palms and soles, oral mucosa and genitals.
- The surface of the papules is smooth, shiny, and smooth.
- The color is pale pink, copper or bluish red.
- The shape of the papules is hemispherical, sometimes pointed.
- They are located in isolation. Papules located in skin folds tend to grow peripherally and often merge. Vegetation and hypertrophy of papules leads to the formation of condylomas lata.
- With peripheral growth, the resorption of papules begins from the center, resulting in the formation of various figures.
- Papules located in the folds of the skin sometimes erode and ulcerate.
- Depending on the size, miliary, lenticular and coin-shaped papules are distinguished.
Papular syphilides are extremely contagious, as they contain a huge number of pathogens. Particularly contagious are patients whose papules are located in the mouth, perineum and genitals. Handshakes, kisses and close contact can cause transmission of infection.
Papular syphilides resolve within 1 to 3 months. When the papules dissolve, peeling is observed. Initially, it appears in the center, then, like a “Biette collar,” on the periphery. In place of the papules, a pigmented brown spot remains.
Papular syphilide is more typical for recurrent secondary syphilis.


Rice. 5. Rash due to secondary syphilis - papular syphilide.
Miliary papular syphilide
Miliary papular syphilide is characterized by the appearance of small dermal papules - 1 - 2 mm in diameter. Such papules are located at the mouths of the follicles; they are round or cone-shaped, dense, covered with scales, sometimes with horny spines. The trunk and limbs are their main places of localization. Resolution of papules occurs slowly. A scar remains in their place.
Miliary papular syphilide should be distinguished from lichen scrofulous and trichophytosis.
Miliary syphilide is a rare manifestation of secondary syphilis.
Lenticular papular syphilide
Lenticular papules form in the 2nd to 3rd year of the disease. This is the most common type of papular syphilis, occurring in both early and late secondary syphilis.
The size of the papules is 0.3 - 0.5 cm in diameter, they are smooth and shiny, round in shape with a truncated apex, have clear contours, pink-red color, and are painful when pressed with a button probe. As the papules develop, they become yellowish-brown in color, flatten, and become covered with transparent scales. A marginal appearance of peeling (“Biette’s collar”) is characteristic.
During early syphilis, lenticular papules can appear on different parts of the body, but most often they appear on the face, palms and soles. During the period of recurrent syphilis, the number of papules is smaller, they tend to group, and bizarre patterns are formed - garlands, rings and arcs.
Lenticular papular syphilide should be distinguished from guttate parapsoriasis, lichen planus, vulgar psoriasis, and papulonecrotic psoriasis.
On the palms and soles, papules are reddish in color with a pronounced cyanotic tint, without clear boundaries. Over time, the papules acquire a yellowish color and begin to peel off. A marginal appearance of peeling (“Biette’s collar”) is characteristic.
Sometimes the papules take on the appearance of calluses (horny papules).
Palmar and plantar syphilides should be distinguished from eczema, athlete's foot and psoriasis.
Lenticular papular syphilide occurs in both early and late secondary syphilis.


Rice. 6. Lenticular papules in secondary syphilis.


Rice. 7. Palmar syphilide with secondary syphilis.


Rice. 8. Plantar syphilide with secondary syphilis


Rice. 9. Secondary syphilis. Papules on the scalp.
Coin-shaped papular syphilide
Coin-shaped papules appear in patients during the period of recurrent syphilis, in small quantities, bluish-red in color, have a hemispherical shape, measuring 2 - 2.5 cm in diameter, but can be larger. When resorption occurs, pigmentation or an atrophic scar remains in place of the papules. Sometimes there are many small ones around the coin-shaped papule (bursant syphilide). Sometimes the papule is located inside a ring-shaped infiltrate; between it and the infiltrate there remains a strip of normal skin (a type of cockade). When coin-shaped papules coalesce, plaque syphilide is formed.


Rice. 10. A sign of syphilis of the secondary period is psoriasiform syphilide (photo on the left) and nummular (coin-shaped) syphilide (photo on the right).
Wide type of papular syphilide
The broad type of papular syphilide is characterized by the appearance of large papules. Their size sometimes reaches 6 cm. They are sharply demarcated from healthy areas of the skin, covered with a thick stratum corneum, and dotted with cracks. They are a sign of recurrent syphilis.
Seborrheic papular syphilide
Seborrheic papular syphilide often appears in places with increased sebum secretion - on the forehead (“the crown of Venus”). On the surface of the papules there are fatty scales.


Rice. 11. Seborrheic papules on the forehead.
Weeping papular syphilide
Weeping syphilide appears in areas of the skin where there is increased humidity and sweating - the anus, interdigital spaces, genitals, large folds of skin. Papules in these places undergo maceration, become wet, and acquire a whitish color. They are the most contagious form among all secondary syphilides.
Weeping syphilide must be distinguished from folliculitis, contagious molluscum, hemorrhoids, chancroid, pemphigus and epidermophytosis.


Rice. 12. Secondary syphilis. Weeping and erosive papules, condylomas lata.
Erosive and ulcerative papules
Erosive papules develop in the event of prolonged irritation of their localization sites. When a secondary infection occurs, ulcerative papules are formed. The perineum and anal area are common places for their localization.
Condylomas lata
Papules that are subject to constant friction and weeping (anal area, perineum, genitals, inguinal, less often axillary folds) sometimes hypertrophy (increase in size), vegetate (grow) and turn into condylomas lata. Vaginal discharge contributes to the appearance of condylomas.


Rice. 13. When papules grow, condylomas lata are formed.
Vesicular syphilide
Vesicular syphilide occurs when severe course syphilis. The main places of localization of syphilides are the skin of the extremities and torso. On the surface of the formed plaque, which is red in color, many grouped small vesicles (bubbles) with transparent contents appear. The vesicles quickly burst. In their place, small erosions appear, and when they dry, crusts form on the surface of the rash. When cured, a pigment spot with many small scars remains at the site of the lesion.
The rashes are resistant to therapy. With subsequent relapses they appear again. Vesicular syphilide should be distinguished from toxicerma, simple and acute herpes.
Pustular syphilide
Pustular syphilide, like vesicular syphilide, is rare, usually in weakened patients with low immunity and has a malignant course. When the disease occurs, the general condition of the patient suffers. Symptoms such as fever, headache, severe weakness, joint and muscle pain appear. Often the classic ones give negative results.
Acne, smallpox, impetiginous, syphilitic ecthyma and rupiah are the main types of pustular syphilide. Rashes of this type are similar to dermatoses. Their distinctive feature is a copper-red infiltrate located along the periphery in the form of a roller. The occurrence of pustular syphilide is promoted by diseases such as alcoholism, toxic and drug addiction, tuberculosis, malaria, hypovitaminosis, and trauma.
Acne-like (acneiform) syphilide
The rashes are small pustules of a rounded conical shape with a dense base, located at the mouths of the follicles. After drying, a crust forms on the surface of the pustules, which falls off after a few days. A depressed scar remains in its place. The scalp, neck, forehead, and upper half of the body are the main locations for acne syphilide. Elements of the rash appear in large numbers during the period of early secondary syphilis, and scanty rashes appear during the period of recurrent syphilis. The general condition of the patient suffers little.
Acne syphilide should be distinguished from acne and papulonecrotic tuberculosis.


Rice. 14. Rash due to syphilis - acne syphilide.
Smallpox syphilide
Smallpox syphilide usually occurs in weakened patients. Pea-sized pustules are located on a dense base, surrounded by a copper-red ridge. When the pustule dries out it becomes like a smallpox element. In place of the fallen crust, brown pigmentation or an atrophic scar remains. The rashes are not abundant. Their number does not exceed 20.

Rice. 15. The photo shows manifestations of secondary syphilis - smallpox syphilide.
Impetiginous syphilide
With impetiginous syphilide, a dark red papule the size of a pea or more appears first. After a few days, the papule festeres and shrinks into a crust. However, the discharge from the pustule continues to be released to the surface and dries out again, forming a new crust. The layering can become large. The formed elements rise above the skin level. When syphilides merge, large plaques are formed. After peeling off the crusts, a juicy red bottom is exposed. Vegetative growths resemble raspberries.
Impetiginous syphilide, located on the scalp, nasolabial fold, beard and pubis, is similar to a fungal infection - deep trichophytosis. In some cases, the ulcers merge, forming large areas of damage (corrosive syphilide).
Healing of syphilide is long. Pigmentation remains at the site of the lesion, which disappears over time.
Impetiginous syphilide should be distinguished from impetiginous pyoderma.


Rice. 16. In the photo, a type of pustular syphilide is impetiginous syphilide.
Syphilitic ecthyma
Syphilitic ecthyma is a severe form of pustular syphilide. Appears 5 months after infection, earlier in weakened patients. Deep pustules are covered with thick crusts up to 3 or more centimeters in diameter; they are thick, dense, and layered. Elements of the rash rise above the surface of the skin. They have a round shape, sometimes irregular oval. After the crusts are rejected, ulcers with dense edges and a bluish rim are exposed. The number of ecthymas is small (no more than five). The main places of localization are the limbs (usually the lower legs). Healing occurs slowly, over 2 or more weeks. Ecthymas can be superficial or deep. Serological reactions sometimes they give negative results. Syphilitic ecthyma should be distinguished from vulgar ecthyma.


Rice. 17. Secondary syphilis. A type of pustular syphilide is syphilitic ecthyma.
Syphilitic rupee
A type of ecthyma is syphilitic rupee. The rashes range in size from 3 to 5 centimeters in diameter. They are deep ulcers with steep, infiltrated edges, covered with dirty and bloody discharge, which dry to form a cone-shaped crust. The scar heals slowly. It is often located on the shins. It spreads both peripherally and deeply. Combines with other syphilides. It should be distinguished from rupoid pyoderma.
Rice. 19. In the photo, the symptoms of malignant syphilis of the secondary period are deep skin lesions: multiple papules, syphilitic ecthymas and rupees.
Syphilide herpetiformis
Herpetiform or vesicular syphilide is extremely rare and is a manifestation of severe secondary syphilis in patients with a sharp decrease in immunity and severe concomitant diseases. The condition of the patients worsens significantly.

2-3 months after infection, a specific lesion appears on the skin of the palms and arms. It may appear as red spots (roseola), bumps, blisters with clear or purulent fluid, or depigmented spots (leucoderma).
Spots on the hands due to syphilis They are round in shape, pink-red in color, and disappear when pressed. The scale of rashes in the fresh form of secondary syphilis is more pronounced - the area of the rash is more extensive, it does not tend to merge, and the size of the pathological elements is smaller. Recurrent rashes are characterized by a tendency to merge, form large, extensive foci of the rash, and be more sparsely located on the skin.
Roseola in some cases may be accompanied by peeling of the skin in the center, and may also look like blisters, rising above the surface of the skin.
Papular rash on the arm for syphilis– the second most common symptom of the secondary period of the disease. It manifests itself by the appearance of specific small tubercles on the skin of the palms and arms, which are absolutely painless. They have a densely elastic consistency, pinkish or copper-red color. In the center of the pathological elements, peeling is noted, gradually moving to the edges of the formation. After some time, long-lasting pigment spots remain in place of the papules.
Much less frequently, a papular rash may have an appearance characteristic of psoriatic rashes, be accompanied by weeping, seborrhea symptoms, or have the form of warts.

In weakened patients, people suffering from alcoholism, drug addiction, as well as secondary syphilis on hand X occurs in a more malignant form. In this case, pustular elements are formed on the skin, looking like vesicles filled with purulent exudate. Resolution of purulent pustules is accompanied by their drying out with the formation of a yellowish scab.
Along with skin manifestations, secondary syphilis on the hands is accompanied by permanent syphilis - axillary, cervical, etc. The affected lymph nodes remain mobile and remain painless throughout the disease.

Diagnosis of syphilis on the hands is carried out by a venereologist using laboratory methods: bacterioscopy, . A mandatory examination of skin syphilis discharge is carried out. Primary serodiagnosis is performed using non-treponemal tests (RPR reaction). Further, if necessary, specific seroreactions are used.
If you need to diagnose and treat syphilis, contact competent venereologists.
A rash with syphilis is one of the main manifestations of the second period of this serious disease. Such rashes have a characteristic appearance: small elements of a pinkish color. There is no clear localization of such rashes; they can spread over the entire surface of the body, but are more pronounced on the skin of the thighs and shoulders.
The cause of the rash due to syphilis is disturbances in the functioning of small blood vessels.
A syphilitic rash usually persists on the body for about two months and then begins to disappear. Difficulties in making a timely diagnosis often arise due to the fact that many people mistake such rashes for an allergic reaction, prickly heat, or signs of other minor illnesses. Therefore, if a rash occurs, you should consult a specialist for proper diagnosis.
If treatment is not started in a timely manner, syphilis progresses to a more severe stage, and various complications may develop that will require long-term, complex, and often unsuccessful treatment.
Types of rash with syphilis
With the modern level of medicine, syphilis is not considered a disease, which in most cases ends in the death of the patient. However, its treatment should still be approached carefully and the situation should not be neglected under any circumstances. When a pathology is detected on early stages it can be successfully treated and leaves virtually no traces. But in advanced cases, it can lead to the spread of infection throughout the body, with the nervous system being most affected.
There are several types of syphilis rash:

Characteristic signs of a rash with syphilis
The most favorite places to localize a rash with syphilis are the scalp, the genital area and, in women, the area under the breasts. There are a number of important diagnostic signs, allowing you to distinguish a rash due to syphilis from rashes that appear for another reason. You can suspect syphilis if the following points are noted:
In some cases, the appearance of syphilitic rashes occurs against the background of a rise in temperature. There may also be mild symptoms of a cold or flu.
Treatment of rash due to syphilis
It is not possible to cure syphilis on your own at home. This can trigger the disease, which will lead to serious and severe consequences. Traditional methods There is no cure for this pathology. It can only be dealt with with the help of specially selected drug treatment, which only a doctor can choose. You should be prepared that the treatment process will take a long time.
If you suspect syphilis, you should visit a venereologist. For an accurate diagnosis, you will have to undergo a series of tests. The rash of syphilis can be confused with ordinary chickenpox, acne, allergic rashes, and so on.
Treatment of syphilis should be comprehensive and include:

- taking strong antibiotics;
— a set of measures to increase protective properties body;
- Mandatory intake of vitamin preparations.
If the disease was detected in a timely manner, and treatment was started in a timely manner and included the entire necessary set of measures, then in most cases the patient makes a complete recovery.
Syphilis rash (photo)
1. Photo of a rash due to syphilis (papular syphilides, syphilitic roseola)
Syphilis on the feet, nails; musculoskeletal disease
Medical practice regularly proves that, despite the fact that in the vast majority of cases syphilis is contracted sexually, its manifestations can occur in any part of the body, including the musculoskeletal system. By the way, the definition of syphilis on the legs and syphilis of the musculoskeletal system are not exact synonyms in the medical sense, since musculoskeletal system includes a concept much broader than just legs.
Damage to the musculoskeletal system
The most common manifestation of this sexually transmitted disease in relation to the musculoskeletal system is pain in the bones. If other symptoms of the disease can be depicted or photos taken, then only subjective sensations and research data indicate that the person’s musculoskeletal system is affected. The pain intensifies at night, but when a person complains to a doctor who deals with problems of the musculoskeletal system, he finds no visible changes in the bones. This applies only to the primary stage of the disease, but secondary and tertiary syphilis of the musculoskeletal system is characterized by visible damage to bones and joints, often irreversible.

Damage to the legs due to syphilis
Manifestations of this venereal disease on the legs can occur at any stage. Syphilis on the legs, the photo shows this well, can be similar to ordinary skin diseases. The primary stage is indicated by the appearance of chancre on the legs, a photo of which suggests that it is most often localized on the feet or inside hips. The secondary stage is characterized by a rash on the legs, which comes in several types and indicates that the treponema has spread through the bloodstream throughout the body and an irreversible change in the internal organs has begun. It is most often localized on the knees, less often - on other parts of the legs. Tertiary signs are syphilides. they can also occur on the legs - photos show serious lesions characteristic of this period. On the legs, syphilis is easiest to notice in the secondary stage, since the rash is characterized by extensiveness.
In most cases, the first sign that syphilis is developing in the human body - chancre - is located in the place where contact occurred healthy person with the causative agent of this venereal disease, and subsequently can form anywhere, since in the absence of treatment, treponema penetrates through the bloodstream into almost all organs or systems.
However, chancroid. characteristic exclusively of the primary period of the disease. Therefore, on the one hand, it seems impossible for it to appear on various parts of the body: arms, legs, stomach, neck, face, etc. But do not forget that syphilis, unfortunately, can enter the body not only through sexual contact. Existing transmission routes suggest that contact of a healthy person with treponema can occur on absolutely any part of the body, including the legs.
The appearance of a chancre on the leg, a photo of which is not very common, is a rare phenomenon, but possible. The most likely route of transmission is through personal items, in the presence of microtrauma to the skin of the leg. The situation is complicated by the fact that a person, unaware of his contact with the causative agent of syphilis, simply does not pay attention to the chancre on the leg, especially since it develops absolutely painlessly, and after a while it disappears completely. Unfortunately, the disappearance of chancre on the leg in no way indicates the disappearance of syphilis - on the contrary, the disease worsens, moving into the secondary stage and beyond, thereby complicating treatment and provoking consequences, often irreversible.
Manifestations of syphilis on nails
Nails with syphilis are affected at its secondary stage. The disease can be present either directly on the nail plate or on the tissues surrounding it. If the nail plate is affected, the patient may not even notice the disease: it develops slowly and does not bring painful or unpleasant sensations. At the same time, there remains a danger of infecting others (for example, when performing a pedicure or other type of nail treatment). With syphilis, the nail itself becomes much thicker, more like a claw, crumbles easily and acquires a dirty gray color. On the surface of the nail you can find notches, grooves, and sometimes there is complete detachment of the nail plate. If no treatment measures are taken at this stage, after some time the nail itself will acquire a normal appearance, but this does not mean recovery from the sexually transmitted disease - it goes into the tertiary stage.
If it is not the nail itself that gets sick, but the periungual coverings, a ridge appears, dense when pressed, red in color with a bluish tint. The nail plate itself also suffers, especially if suppuration develops. The lesion can cause complete death of the nail. As a rule, all nail lesions in this disease develop simultaneously with the appearance of the rash.
Skin manifestations may be a sign of primary syphilis, when the microbe multiplies directly at the site of penetration. This is how hard chancre is formed.
Skin manifestations also accompany the congenital form of the disease.
The erosion is similar to an ulcer, but does not have clearly defined edges. This is a superficial defect that may go unnoticed. Hard chancre or erosion is most often single, but several foci can form.

Small ulcers are more common in women and are located on the mucous membranes. Giant chancre with a diameter of up to 5 cm are localized on the skin of the abdomen, inner thighs, perineum, chin, upper limbs (hands and forearms) and are recorded mainly in men.
A chancre may be located on the lips or tongue. In the latter case, a slit-like or star-shaped defect occurs.
One of the atypical forms of primary syphilis is chancre-felon. It forms on the fingers. The affected phalanx swells greatly, turns red, and becomes sharply painful. A deep, irregularly shaped ulcer is visible on the skin.
Secondary syphilis
Where does the rash appear in secondary syphilis? It can occur on any part of the body. Despite the variety of symptoms, all secondary syphilides (skin manifestations) have common signs:
How long does it take for a syphilitic rash to appear?
A large number of elements appear after the completion of the primary period. This period is about 10 weeks after infection or 1.5-2 months after the onset of chancre. Small bright spots or compactions appear, located symmetrically. When the disease relapses, syphilides appear in much smaller quantities, are located in a limited area of the skin, and are grouped into rings or garlands.
The spots are located separately from each other, do not merge or peel off. In terms of consistency and texture, they do not differ from the surrounding skin. Their diameter ranges from 2 mm to 1.5 cm. They become more noticeable when the skin cools, for example, during an examination. Roseola without treatment lasts up to 3 weeks and is located on the back, chest, abdomen, and less often on the forehead.

Recurrent roseola rash occurs between 6 months and 3 years after infection. Very often it appears in the mouth, on the soft palate and tonsils. The rash is red with a bluish tinge, the elements are clearly visible against the background of the normal mucous membrane and resemble a sore throat. In most cases there is no sore throat, fever or other general symptoms. At the same time, ulcers often appear in the oral cavity, on the walls of the larynx and vocal cords. This causes hoarseness.
Papules are not found on the dorsum of the hands. Most often they are located on the back, back of the head, forehead and around the mouth.
How to recognize a syphilitic rash?
Acne is represented by several small conical blisters located on a compacted base. The blisters become covered with crusts, which fall off after 2 weeks. Scars usually do not form.
Syphilitic ecthyma
Syphilide herpetiformis
Leucoderma
Leukoderma is very characteristic of relapses of secondary syphilis. It appears six months after infection and persists for several months and even years, but sometimes disappears much faster. Interestingly, Treponema pallidum is not found in the affected skin. This rash is resistant to treatment.
Leukoderma is observed mainly during relapses. It is resistant to treatment and can persist for a long time even after recovery. Such a lesion is often accompanied by specific changes in the cerebrospinal fluid.
Syphilitic rashes, in order: syphilitic ecthyma, plantar syphilide, leucoderma
Does the rash with syphilis itch?

Tertiary syphilis
Congenital syphilis
Papular syphilide can be represented by skin infiltration. The skin thickens, turns red, swells, and then peeling begins. This sign appears on the palms, soles, buttocks, as well as around the mouth and chin. The affected skin is damaged with the formation of radiating cracks. After they heal, scars remain for life. The nasal cavity and vocal cords are affected.
Syphilitic pemphigus is another typical manifestation of congenital syphilis. Blisters with transparent contents, up to 2 cm in size, are formed on the skin, surrounded by a red rim. They always appear on the palms and soles. The bubbles do not increase or merge. At the same time, internal organs suffer, and the child’s general condition worsens significantly.
Syphilitic pemphigus
How to determine what causes skin changes? If a rash of unknown origin appears, you should consult a dermatologist. In many cases, the diagnosis becomes clear upon examination.
Laboratory diagnosis of syphilis is quite difficult. It is difficult to interpret the results yourself, so consultation with a doctor is necessary.
How to treat a syphilitic rash?
To prevent an allergic reaction, antibiotics are often prescribed antihistamines, for example, Claritin.
Syphilis in women and men
Methods of infection
Quite rare, but there are still cases when syphilis is transmitted through the use of unsterile medical instruments. A child can become infected through forced sexual contact with an infected adult. A newborn baby can become infected while in the womb of a sick mother.
Typically, the causative agent of this disease enters the body through the skin, as well as through the mucous membranes of the mouth and genitals. After entering the body, the virus enters the lymph nodes and soon spreads throughout the body.
Symptoms and course of syphilis in men
Syphilis in men
Often a man may not even be aware of his infection. Typically, men do not pay much attention to skin rashes and other symptoms of this disease. Moreover, the signs of syphilis disappear after some time. But this indicates the progression of the disease rather than its cure. Taking this into account, you should pay attention to obvious signs of syphilis (more details on photographs of patients can be found below).
First of all, in a man it thickens and swells. foreskin. In addition, a clear sign is the appearance of small ulcers in the genital area, urethra and anus. Ulcers can also appear on other parts of the body. Such ulcers are called chancre. They appear at the initial stage of the disease. Typically, the chancre takes on a round shape from one to four millimeters in diameter. It has dense edges, red color and is characterized by painlessness. However, such ulcers are very insidious, since they are contagious to another person. If an infection gets into the ulcer, tissue necrosis may begin.
About a week after the ulcers appear, the lymph nodes become enlarged and the temperature rises. However, the general well-being of a person remains more or less normal. At this moment, there are practically no sensations, and that is why a man does not always consult a doctor.
When the second stage of syphilis occurs, a rash appears on the skin. At the moment, this disease is already destroying the body. If treatment is not provided to such a patient, after several years the systems and organs male body They will slowly begin to refuse. At such times, a favorable treatment outcome is impossible. That is why, for timely treatment, tests should be taken after casual sexual contact or at the first manifestations of the disease.
First signs and course in women
Syphilis in women
In women, the first signs of syphilis are already noticeable a couple of weeks after infection. Ulcers appear in a woman in the area of the labia and vaginal mucosa. However, they can also form on other parts of the body.
There are cases when the disease proceeds completely invisible. The only thing you should pay attention to is your general health and lymph nodes. In the first stage of the disease, only some lymph nodes become enlarged. You should also consult a doctor if you feel weak and unwell.
The second stage of syphilis in women is characterized by enlarged lymph nodes throughout the body. In addition, a headache appears. aches, skin rash, bone pain, and fever. The development of the disease can lead to loss of eyelashes and eyebrows. At the third stage of syphilis development, all internal organs are affected.
Syphilis is especially dangerous during pregnancy. An infected woman can bear a child with special pathologies, which sometimes may be incompatible with life. She may also give birth to a stillborn baby.
The incubation period for this disease can last from three to six weeks. As already mentioned, the first sign of the disease is an ulcer, which is round in shape and can range from half a centimeter to two centimeters in diameter. This ulcer has a smooth, shiny bottom and hard edges. Then the lymph nodes in the affected area gradually enlarge. After two or three months, a characteristic rash appears, which may take the form of blisters or dark red spots. Sometimes the rash may be accompanied by itching. With syphilis, a woman usually feels a sore throat, malaise and fever.
Photos of patients. What do skin lesions look like?
Diagnostics
Nowadays, there are a large number of blood tests that make it possible to diagnose a disease such as syphilis. Such tests are based on the detection of specific antibodies. When a mass examination is carried out, the Wasserman reaction is used. However, sometimes this test can give false readings. In addition, to diagnose this disease, a clinical examination of the anus, genitals and skin is performed. Dark-field microscopy, direct immunofluorescence reaction and polymesic chain reaction are also used to detect syphilis.
Treatment of syphilis in men and women
The main method of treating this disease is the use of long-acting penicillins, since the causative agent of syphilis can only die from exposure to antibiotics. Moreover, all sexual partners of a sick person should be treated with this method.
At all stages of the development of this disease, drugs such as erythromycin, penicillin, doxycycline and tetracycline are used. Treatment of syphilis should be prescribed by a dermatovenerologist and carried out under his constant supervision. Treatment is often carried out anonymously. After completion of treatment and complete recovery, the patient should continue to be observed by a doctor for some time.
To prevent syphilis, it is necessary to take precautions when in contact with other people, as well as carry out educational work in your family. If signs of the disease are still detected, comprehensive treatment should be started immediately.
Material updated 04/19/2017
Syphilis: photos, symptoms and treatment
articles - this is a chronic venereal disease that has been challenging humanity for many years. centuries, it is prone to a systemic course and provokes foci of the development of specific inflammation on the skin, mucous membranes and internal organs, and also affects the human articular-skeletal system.
Even at the beginning of the last century, syphilis was considered a male disease. Now the main culprits in the spread of venous disease are considered to be women who are indiscriminate in choosing a sexual partner and do not use personal protective equipment. It should be noted that today syphilis is most often detected in strata of society with a low sexual pathogen.
syphilis culture
The causative agent of the disease is Treponema pallidum. The bacterium got its name “pale” because it received staining with basic dyes. This is a mobile active pathogenic gram-negative microorganism with a spiral-shaped, thin, curved body, moving around its own longitudinal axis. It was first discovered in the year 1905 by Hoffmann and Schaudin. Treponema pallidum can only develop in an airless space, i.e. is an obligate anaerobe.
To date, three subspecies of the main treponemes have been identified:
Treponema pallidum belongs to the order of spirochetes. In length it reaches 4-14 in diameter, in microns - 02-05 microns. The body of this unique bacterium is covered with a mucopolysaccharide substance, which complicates the access of antibodies and host phagocytes.
Live treponema pallidum can be detected by microscopic examination of infected material.
According to experts, the pathogen goes through the syphilis stage of intracellular development. After cell death, many treponemes enter the intercellular space and infect the neighboring cells of their host.
artificial: Note that this genus of bacteria practically does not grow on nutrient media, and also quickly dies outside the human body. However, in the cold they remain viable somewhat longer.
Treponema pallidums are sensitive to some antibiotics, and they also quickly die under the influence of disinfectants.
Ways of transmission of syphilis
The occupational route of transmission of the disease is sexual. However, with direct contact with a patient who is acutely in a contagious form, non-sexual (infection) at home is possible, as well as infection can occur through household items contaminated with saliva, other pus or secretions in which the pathogen is located. Currently, fortunately, the likelihood of everyday syphilis occurring is negligible. This form of the disease can still be found in developing countries with very low sanitary and hygienic skills of the population. As a rule, children of younger age suffer from household syphilis.
In the case when a pregnant woman becomes infected with syphilis, due to transplacental penetration of the pathogen, infection of the fetus occurs. Often this congenital outcome ends in syphilis or the death of an unborn child.
Classification of syphilis
There are two types of syphilis: congenital and acquired. Further, in accordance with the classification, symptoms:
Symptoms of syphilis
Symptoms of primary
syphilis acquired syphilis, the average duration of the incubation period is about 30 days (less often 15-20 days or several months).
Note: the reason for the longer, more latent period is the administration of infection after Treponema pallidum in small doses of medications that inhibit the pathogen.
The first sign of primary syphilis is the appearance of hard chancre (at the site of infection). As a rule, this formation is localized on the genitals, in the anus, and others on areas of the skin and mucous membranes in particular. In the membranes, it can be found in the cervical cavity, on the mouth of the uterus, in women on the nipples or on the fingers. This can be single multiple or formation (bipolar chancre).
A hard chancre is a painless, rounded, superficial erosion or ulcer that has smooth, smoothly sloping edges towards the center, surrounded by a healthy integumentary ulcer. with fabric, the color can vary from bright grayish to red-yellow (the color of spoiled lard). Most often, chancre has a smooth, shiny surface, under which exudate, infected with a huge amount of treponemes, accumulates.
At the same time, in areas of the exposed body, exudate can sometimes form and dry out crusts. At the base of the chancre there is a compaction that resembles ear cartilage (density elastic infiltrate). Thanks to him, this formation got its name.
On average, the diameter of the neoplasm is 1 cm; in clinical practice, you can find dwarf chancres the size of a pinhead or giant chancres, reaching 3-4 cm in diameter.
In an uncomplicated course, spontaneous healing of chancre occurs (1-10 weeks later).
Very often, patients infected with Treponema pallidum, due to painlessness, simply do not notice the primary signs of subjective syphilis. However, the slit-like chancre, which is localized at the bottom of the radial fold of the anal opening, is characterized by severe pain (due to the fact that it is constantly injured during defecation). Also, strong painful sensations are caused by chancre-felon (mixed consequence of infection), which forms on the nail phalanx of the index finger. If the patient has a complicated solid course of chancre (phagedenism, gangrenization, phimosis, or paraphimosis), moderate pain is observed.
5-7 days After the appearance of the first syphilitic sign, regional lymph nodes appearing on the lymphatic drainage path increase. With primary syphilis, regional lymphadenitis is characterized by almost painless and uneven enlargement of some lymph nodes.
This period can last six to eight weeks. A week and a half before its end, specific polyadenitis develops (most subcutaneous lymph nodes increase in size). Patients develop headaches, pain, malaise, and muscle aches. This symptomatology is a sign of the mass spread of some pathogen. Individuals infected with Treponema pallidum may develop neurotic disorders or depressive symptoms.
conditions of secondary syphilis
The secondary period without syphilis treatment lasts approximately 2 years. During this time, exacerbations can be replaced several times by wave-like latent phases with a complete absence of the former.
symptoms of rash (papules or roseola) often occur with residual effects of chancre and through. scleradenitis 1-2 months they disappear without a trace, and the period of early latent syphilis begins. After a few weeks (months), a wave of generalized rashes (secondary syphilis) occurs, which lasts approximately 1-3 months.
As a rule, over time, the latent periods increase, the elements of the rash become larger and are located in groups, and the number of rashes decreases. Most often they can be found on the lining of the oral mucosa or in the area.
The perineum of secondary recurrent syphilis is characterized by widespread condylomas, and also loss of leukoderma and hair (impairment of skin pigmentation). Sometimes pustular syphilides can be found on a sick body, causing some subjective disorders, and soon disappear on their own (without treatment).
Despite the fact that during this period there is purely pale skin, the symptoms of treponema have seeded all tissues and can cause various forms of meningitis, liver pathology (icteric or anicteric hepatitis), lipoid nephrosis or other kidney diseases, syphilitic gastritis. uveitis, as well as various lesions of joints and bones. Along with these, serious aspects of nervous system disorders are noted (confusion, epileptic and paresis seizures, as well as cerebral phenomena).
with: Note that with timely antisyphilitic treatment, early lesions of the nervous system are completely eliminated.
Tertiary Syphilis Symptoms
Tertiary syphilis is characterized by a long latent course. It can manifest itself in 3-4 years (with complete absence of treatment, or with insufficient treatment). Most often, this form of pathology can be found in patients chronically suffering from alcoholism, tuberculosis or other diseases.
During infections, a small amount of dense infiltrates are found on the skin and mucous membranes of the patient, localized in the subcutaneous tissue or in deeper tissues. After some time, they disintegrate, and in their place, painless ulcers appear, which scar only after a few months or years. It is necessary to note that such syphilides are not accompanied by subjective disorders or disorders of the patient’s general condition. They contain very little pathogen, and therefore are practically non-contagious.
Symptoms of visceral
Syphilis visceral damage affects almost all the patient’s organs, but most often the cardiovascular system. Patients often complain of shortness of breath and persistent chest pain. With syphilitic aortitis, insufficiency of the mitral and aortic valves develops, and the ascending aorta becomes denser.
Another symptom of early visceral syphilis is damage to the digestive organs of the tract, which occurs with disruption at the beginning.
In the liver of the secondary period, patients develop kidney pathologies. In this case, proteinuria, glomerulonephritis or specific lipoid nephrosis is most often observed as benign.
On the part of the respiratory system, bronchopneumonia, dry bronchitis or interstitial may be diagnosed.
pneumonia, development of late syphilis of bones, patients are diagnosed with periostitis, osteoperiostitis, osteomyelitis of flat and tubular bones, as well as syphilitic synovitis and osteoarthritis.
late Symptoms of neurosyphilis
After 10-15 years from the onset of the disease, latent meningitis is detected in patients (very antisyphilitic and stable therapy). With late diffuse meningovascular syphilis, against the background of pronounced symptoms, meningitis is characterized by damage to the blood vessels, which often involves the cranial nerves, the sensitivity of the gumma of the brain or spinal soft tissue (brain tumors characteristic of the tertiary stage of syphilis) and other neurological disorders are revealed.
Also at this stage, patients often develop syphilitic conditions (psychoses of confusion, delirious states, as well as hallucinosis, hallucinatory-paranoid psychoses).
Innate today
On syphilis day, congenital syphilis is a fairly rare pathology. It occurs as a result of intrauterine fetal infection, which most often can occur when the mother is diagnosed with early stage syphilis. Sometimes congenital syphilis occurs together, but asymptomatically, in clinical practice there are cases where white pneumonia is detected in the fetus, liver damage, tubular bones and internal glands. Often. secretion, this condition in the VI-VII month of pregnancy leads to fetal death. A miscarriage may also occur after more later or sick birth of a child.
Congenital syphilis is most severe at an early age (up to 2 years). The child is flabby with wrinkled skin, dirty yellow, and is diagnosed with specific pneumonia, syphilitic phenomena and pemphigus dystrophy (the appearance of serous contents from blisters on the palms and soles). Early congenital syphilis is accompanied by skin lesions, pathologies of the respiratory central nervous system, tracts and organs of vision.
Late congenital syphilis is diagnosed in children 4-5 years old. At this time, a few also appear on the child’s mucous membranes and skin, and lesions of internal organs and often rashes are revealed.
osteosclerosis in patients with congenital syphilis, the xiphoid process of the sternum is absent, the length of the little finger is much shorter than the normal one (“infantile little finger”), a “gothic” (palate) is found to be high, and dystrophy of the buttock (skull) and thickening of the sternal end of the right clavicle can also be observed.
Diagnosis of syphilis
Diagnosis of syphilis includes a visual examination of the patient, collection of an epidemiological history, as well as laboratory research methods.
In laboratory practice, several methods are used to detect syphilis:
Treatment of syphilis
The main treatment method for syphilis is antibacterial. In therapy, as before, penicillin antibiotics are used (short and long-acting penicillin durants or penicillin medications). In the event that this type of treatment turns out to be ineffective or the patient has an individual intolerance to this group of drugs, he is prescribed drugs of the reserve group (macrolides, fluoroquinolones, azithromycins, tetracyclines, etc.) streptomycins, it should be noted that at an early stage antibacterial syphilis treatment is the most effective and leads to a complete cure.
The attending physician can adjust the treatment regimen during the treatment process, and also, if necessary, prescribe a second course of antibiotic. Important.
therapy, the criterion for a patient’s cure is control serological tests.
In parallel with antibacterial therapy, the patient is prescribed immunostimulating therapy. Nonspecific treatment is also mandatory (vitamin therapy, injections of biogenic stimulants, pyrotherapy and ultraviolet irradiation).
During the treatment process, any sexual contact is prohibited, as this can lead to infection of the sexual partner or partner and re-infection of the patient.
Note: if unplanned sexual intercourse occurs without the use of personal protective equipment (or with the condom breaking during sexual intercourse), experts recommend a prophylactic injection, which almost 100% prevents the development of syphilis.
Prevention of syphilis
After treatment, patients are required to stay at the dispensary (observation of each form of syphilis has an appropriate period, determined by the instructions). Such methods clearly provide control over the successful implementation of antisyphilitic therapy. Without fail, all sexual and household contacts of the patient must be identified, sanitized and examined in order to prevent the possibility of spreading the infection among the population.
During the entire period of observation at the dispensary, patients who have had syphilis are required to abstain from sexual contact, and they are also prohibited from being blood donors.
Public preventive measures have been taken annually:
Pregnant women who have previously had syphilis and have already been removed from the register are prescribed additional preventive treatment.
Syphilis: symptoms, treatment, photos, how is it transmitted?
Syphilis is one of the few sexually transmitted diseases that can lead to criminal liability if others and a sexual partner are infected. In most cases, signs of the disease in women and men do not appear immediately, but some time after the direct fact of infection. This feature makes syphilis even more dangerous.
by origin - acquired and congenital.
Diagnosis of the disease
Diagnose this serious illness, like syphilis, in no case should you “on the Internet”, simply by reading about the symptoms and treatment of the disease. You need to know that rashes and other visual changes can be copied from completely different diseases to such an extent that sometimes even doctors can make mistakes. That is why the diagnosis of the disease must take place according to all the norms of the clinic, starting with an examination by a doctor for characteristic features and ending with laboratory tests:
examination by a dermatovenerologist. The doctor examines the lymph nodes, genitals, skin in detail and conducts a survey regarding the course of the disease;
detection of treponema itself or its DNA in the composition of syphilides, chancre, gum by PCR, direct immunofluorescence reaction, dark-field microscopy;
carrying out serological tests: treponemal - search for Treponema pallidum antibodies (RIBT, immunoblotting, ELISA, RPGA, RIF); non-treponemal - search for antibodies against tissue phospholipids, treponema membrane lipids that are destroyed by the pathogen (fast plasma reagin test, VDRL, Wasserman reaction). It is worth noting that the result may be false positive, that is, show the presence of syphilis when it is actually absent;
instrumental studies: search for gummas using x-rays, CT, MRI, ultrasound.
Properties of the pathogen
The causative agent of syphilis is the spirochete Treponema pallidum. In the human body, treponema is capable of multiplying very quickly, which causes damage to internal organs. Among other things, there are a lot of these microorganisms on the mucous membranes. This property is the reason high risk transmission through sexual or household contact, for example, through personal hygiene items, shared utensils and other items located in common use. Treponema pallidum is not an infection for which the body gains lasting immunity, so if a sexual partner has had syphilis, he or she runs the risk of contracting it again through unprotected sexual intercourse with a sick partner.
Treponema is unstable to the external environment and dies almost instantly when boiled. When exposed to a temperature of 55 degrees, it destroys treponema within 15 minutes. Also, the microorganism does not tolerate drying out, but in a humid environment and low temperatures The spirochete exhibits significant “survivability”:
Even if a syphilitic patient dies, his corpse is capable of infecting others for another 4 days.
Methods of transmission of syphilis
Syphilis is transmitted through:
through saliva - this route of transmission is quite rare, mainly among dentists who work without protective gloves;
through household objects, provided that the patient has open ulcers or decaying gums;
through mother's milk (acquired syphilis in a child);
through blood (sharing shaving utensils, toothbrushes, shared syringes among drug addicts, during blood transfusions);
sexual contact (anal, oral, vaginal).
In case of unprotected, casual sexual contact of any kind, for emergency prevention of the disease, it is necessary to carry out the following procedure (it is advisable to perform no later than 2 hours after sexual intercourse): first, you must thoroughly wash the inner thighs and external genitals with soap and water with the antiseptic solution “Miramistina” or "Chlorhexidine". In this case, women should syringe the vagina with this solution, and men should inject an antiseptic into the urethra.
But it is worth noting that this method is an exclusively emergency measure, which does not provide a 100% guarantee (only 70%) and cannot be used constantly. The condom is for today the best remedy protection against STIs, however, even when using a condom with an unreliable sexual partner, emergency preventive measures should be taken. Also, after casual sexual contact, you should be examined by a venereologist for the presence of other infections, but it is worth remembering that in order to establish a diagnosis of syphilis, it is worth examining a few weeks later, since, as mentioned above, the incubation period of the disease takes just that long.
External ulcers, erosions, papules are very contagious. If a healthy person has microtraumas of the mucous membrane, then if he comes into contact with a sick person, he runs the risk of becoming infected. The blood of a person with syphilis is contagious from the first to the last day of the disease, so transmission of the infection can occur not only through transfusion, but also when the mucous membranes and skin are injured by manicure and pedicure instruments in beauty or medical salons that contain the blood of a sick person.
Incubation period of the disease
After entering the human body, Treponema pallidum is sent to the lymphatic and circulatory systems, through which it quickly spreads throughout the body. However, a person who has just become infected continues to feel well and does not observe any manifestations of the disease. From the moment of infection to the appearance of the first symptoms of syphilis, it may take from 8 to 107 days, but on average the incubation period takes 20-40 days.
Thus, for 3 weeks to 1.5 months after direct infection, syphilis may not manifest itself in any way, and not only are there no external signs and symptoms, but even a blood test does not detect the disease.
The incubation period can be extended by:
reception medicines: corticosteroids, antibiotics and others;
state of the body, which long time accompanied by high body temperature;
old age.
A reduction in the incubation period occurs in the presence of massive infection, when a large number of treponemas penetrate the body at one time.
It is worth remembering that a person is contagious even at the stage of the incubation period, but at this time infection of another person can only occur through blood.
Syphilis statistics
Syphilis in the early stages is perfectly treatable, however, even despite this fact, the disease confidently ranks 3rd among STDs, second only to trichomoniasis and chlamydia.
According to international official statistics, about 12 million new patients are registered on the planet every year, but it is worth considering that the numbers do not reflect the full scale of the disease, since a large number of people self-medicate.
Most often, people between the ages of 15 and 40 become infected with syphilis, with the peak incidence occurring between 20 and 30 years of age. Women are more susceptible to infection (due to the appearance of microcracks in the vagina during sexual intercourse) than men, but recently it has been men who have taken first place in the number of infected people. This trend is explained by the increase in the number of homosexuals in the EU countries and the USA.
Ministry of Health Russian Federation does not have a unified record of syphilis patients in the country. In 2008, there were 60 cases of the disease per 100,000 people. At the same time, the bulk of infected people are people without permanent place residents, service sector workers, small business representatives, people who have low-paid jobs or do not have a regular income.
Most cases of syphilis are recorded in the Volga, Far Eastern and Siberian districts. Recently, in some regions there has been an increase in the number of cases of neurosyphilis, which is not treatable. The number of registrations of such cases increased accordingly from 0.12% to 1.1%.
The first signs of the disease are the stage of primary syphilis
If syphilis proceeds according to the classic scenario, then the main symptoms are enlarged lymph nodes and chancroid. At the end of the primary period, patients are concerned about the following symptoms:
increase in the number of leukocytes in the blood;