It is a secret that the organs of vision. Human eye and vision. How Visible Image Is Created
Anatomy is the first science, without it there is nothing in medicine.
Old Russian handwritten medical book according to the list of the 17th century.
A doctor who is not an anatomist is not only useless, but also harmful.
E. O. Mukhin (1815)
The human visual analyzer belongs to the sensory systems of the body and, in anatomical and functional terms, consists of several interconnected, but different structural units (Fig. 3.1):
Two eyeballs located in the frontal plane in the right and left eye sockets, with their optical system that allows focusing on the retina (actually the receptor part of the analyzer) images of all environmental objects located within the clear vision area of each of them;
Systems for processing, encoding and transmitting perceived images through neural communication channels to the cortical section of the analyzer;
Auxiliary organs, similar for both eyeballs (eyelids, conjunctiva, lacrimal apparatus, oculomotor muscles, orbital fascia);
Life support systems of the analyzer structures (blood supply, innervation, intraocular fluid production, regulation of hydro- and hemodynamics).
3.1. Eyeball
Human eye (bulbus oculi), approximately 2/3 located in
cavity of the orbits, has not quite the correct spherical shape. In healthy newborns, its dimensions, determined by calculations, are (on average) 17 mm along the sagittal axis, 17 mm transverse and 16.5 mm vertical. In adults with a commensurate refraction of the eye, these figures are 24.4; 23.8 and 23.5 mm respectively. The mass of the eyeball of a newborn is up to 3 g, an adult - up to 7-8 g.
Anatomical landmarks of the eye: the anterior pole corresponds to the top of the cornea, the posterior pole - to its opposite point on the sclera. The line connecting these poles is called the outer axis of the eyeball. The straight line, mentally drawn to connect the posterior surface of the cornea with the retina in the projection of the indicated poles, is called its internal (sagittal) axis. Limb - the place of transition of the cornea to the sclera - is used as a guide for accurate localization of the detected pathological focus in the clock display (meridian indicator) and in linear quantities, which are an indicator of distance from the point of intersection of the meridian with the limb (Fig. 3.2).
In general, the macroscopic structure of the eye seems, at first glance, deceptively simple: two integumentary (conjunctiva and vagina
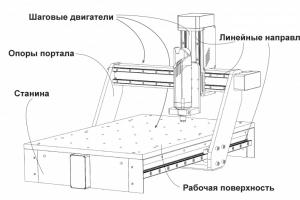
Rice. 3.1. The structure of the human visual analyzer (diagram).
eyeball) and three main membranes (fibrous, vascular, reticular), as well as the contents of its cavity in the form of anterior and posterior chambers (filled with aqueous humor), the lens and the vitreous body. However, the histological structure of most tissues is quite complex.
The fine structure of the membranes and optical media of the eye is presented in the relevant sections of the textbook. This chapter provides an opportunity to see the structure of the eye as a whole, to understand
functional interaction of individual parts of the eye and its appendages, features of blood supply and innervation, explaining the occurrence and course of various types of pathology.
3.1.1. Fibrous membrane of the eye
The fibrous membrane of the eye (tunica fibrosa bulbi) consists of the cornea and sclera, which, according to the anatomical structure and functional properties,

Rice. 3.2. The structure of the human eyeball.
properties differ sharply from each other.
Cornea(cornea) - anterior transparent part (~ 1/6) of the fibrous membrane. The place of its transition to the sclera (limb) has the form of a translucent ring up to 1 mm wide. Its presence is explained by the fact that the deep layers of the cornea extend posteriorly somewhat further than the anterior ones. Distinctive qualities of the cornea: spherical (radius of curvature of the anterior surface ~ 7.7 mm, posterior 6.8 mm), mirror-shiny, devoid of blood vessels, has a high tactile and pain, but low temperature sensitivity, refracts light rays with a power of 40.0-43.0 diopters.
The horizontal diameter of the cornea in healthy newborns is 9.62 ± 0.1 mm, in adults it is
blinks 11 mm (vertical diameter is usually less than ~1 mm). In the center, it is always thinner than on the periphery. This indicator correlates with age: for example, at 20-30 years old, the thickness of the cornea is 0.534 and 0.707 mm, respectively, and at 71-80 years old, 0.518 and 0.618 mm.
With closed eyelids, the temperature of the cornea at the limbus is 35.4 °C, and in the center - 35.1 °C (with open eyelids - 30 °C). In this regard, mold growth is possible in it with the development of specific keratitis.
As for the nutrition of the cornea, it is carried out in two ways: due to diffusion from the perilimbal vasculature formed by the anterior ciliary arteries, and osmosis from the moisture of the anterior chamber and lacrimal fluid (see Chapter 11).
Sclera(sclera) - an opaque part (5/6) of the outer (fibrous) shell of the eyeball 0.3-1 mm thick. It is thinnest (0.3-0.5 mm) at the equator and at the point where the optic nerve leaves the eye. Here, the inner layers of the sclera form a cribriform plate, through which the axons of retinal ganglion cells pass, forming the disc and the stem of the optic nerve.
Scleral thinning zones are vulnerable to increased intraocular pressure (development of staphylomas, excavation of the optic disc) and damaging factors, primarily mechanical (subconjunctival ruptures in typical places, usually in areas between the attachment sites of extraocular muscles). Near the cornea, the thickness of the sclera is 0.6-0.8 mm.
In the area of the limbus, three completely different structures merge - the cornea, sclera and conjunctiva of the eyeball. As a result, this zone can be the starting point for the development of polymorphic pathological processes - from inflammatory and allergic to tumor (papilloma, melanoma) and associated with developmental anomalies (dermoid). The limbal zone is richly vascularized due to the anterior ciliary arteries (branches of the muscular arteries), which, at a distance of 2-3 mm from it, give branches not only into the eye, but also in three more directions: directly to the limbus (form the marginal vascular network), episclera and adjacent conjunctiva. Around the circumference of the limbus there is a dense nerve plexus formed by long and short ciliary nerves. Branches depart from it, which then enter the cornea.
There are few vessels in the sclera tissue, it is almost devoid of sensitive nerve endings and is predisposed
to the development of pathological processes characteristic of collagenoses.
6 oculomotor muscles are attached to the surface of the sclera. In addition, it has special channels (graduates, emissaries). Through one of them, arteries and nerves pass to the choroid, and through others, venous trunks of various calibers exit.
On the inner surface of the anterior edge of the sclera there is a circular groove up to 0.75 mm wide. Its posterior edge protrudes somewhat anteriorly in the form of a spur, to which the ciliary body is attached (the anterior ring of attachment of the choroid). The anterior edge of the groove borders on the Descemet's membrane of the cornea. At the bottom of it at the posterior edge is the venous sinus of the sclera (Schlemm's canal). The rest of the scleral recess is occupied by the trabecular meshwork (reticulum trabeculare) (see Chapter 10).
3.1.2. Vascular membrane of the eye
The choroid of the eye (tunica vasculosa bulbi) consists of three closely related parts - the iris, the ciliary body and the choroid.
iris(iris) - the anterior part of the choroid and, unlike its other two sections, is located not parietal, but in the frontal plane with respect to the limbus; has the shape of a disk with a hole (pupil) in the center (see Fig. 14.1).
Along the edge of the pupil is an annular sphincter, which is innervated by the oculomotor nerve. The radially oriented dilator is innervated by the sympathetic nerve.
The thickness of the iris is 0.2-0.4 mm; it is especially thin in the root zone, i.e., on the border with the ciliary body. It is here that with severe contusions of the eyeball, its detachment (iridodialys) can occur.
Ciliary (ciliary) body(corpus ciliare) - the middle part of the choroid - is located behind the iris, therefore it is not available for direct examination. The ciliary body is projected onto the surface of the sclera in the form of a belt 6-7 mm wide, starting at the scleral spur, i.e., at a distance of 2 mm from the limbus. Macroscopically, two parts can be distinguished in this ring - a flat (orbiculus ciliaris) 4 mm wide, which borders on the dentate line (ora serrata) of the retina, and a ciliary (corona ciliaris) 2-3 mm wide with 70-80 whitish ciliary processes (processus ciliares ). Each part has the form of a roller or plate about 0.8 mm high, up to 2 mm wide and long.
The inner surface of the ciliary body is connected with the lens through the so-called ciliary girdle (zonula ciliaris), consisting of many very thin vitreous fibers (fibrae zonulares). This girdle acts as a ligament that suspends the lens. It connects the ciliary muscle with the lens into a single accommodative apparatus of the eye.
The vascular network of the ciliary body is formed by two long posterior ciliary arteries (branches of the ophthalmic artery) that pass through the sclera at the posterior pole of the eye, and then go into the suprachoroidal space along the 3 and 9 o'clock meridians; anastomose with branches of the anterior and posterior short ciliary arteries. Sensitive innervation of the ciliary body is the same as that of the iris, motor (for different portions of the accommodative muscle) - from the oculomotor nerve.
choroid(chorioidea), or the choroid itself, lines the entire posterior sclera from the dentate line to the optic nerve, is formed by the posterior short ciliary arteries
riami (6-12), which pass through the sclera at the posterior pole of the eye.
The choroid has a number of anatomical features:
It is devoid of sensitive nerve endings, therefore, the pathological processes developing in it do not cause pain;
Its vasculature does not anastomose with the anterior ciliary arteries, as a result, with choroiditis, the anterior part of the eye remains intact;
An extensive vascular bed with a small number of efferent vessels (4 vorticose veins) contributes to slowing down blood flow and settling pathogens of various diseases here;
It is organically connected with the retina, which, as a rule, is also involved in the pathological process in diseases of the choroid;
Due to the presence of the perichoroidal space, it easily exfoliates from the sclera. It is kept in a normal position mainly due to outgoing venous vessels that perforate it in the equatorial region. The stabilizing role is also played by the vessels and nerves penetrating the choroid from the same space (see Section 14.2).
3.1.3. Inner (sensitive) membrane of the eye
Inner lining of the eye retina(retina) - lines the entire surface of the choroid from the inside. In accordance with the structure, and hence the function, two parts are distinguished in it - the optical (pars optica retinae) and the ciliary-iris (pars ciliaris et iridica retinae). The first is a highly differentiated nervous tissue with photoreceptors that perceive
providing adequate light beams with a wavelength of 380 to 770 nm. This part of the retina extends from the optic disc to the flat part of the ciliary body, where it ends with a dentate line. Further, in the form reduced to two epithelial layers, having lost its optical properties, it covers the inner surface of the ciliary body and the iris. The thickness of the retina in different areas is not the same: at the edge of the optic disc 0.4-0.5 mm, in the region of the foveola of the macula 0.07-0.08 mm, at the dentate line 0.14 mm. The retina is firmly attached to the underlying choroid only in a few areas: along the dentate line, around the optic nerve head, and along the edge of the macula. In other areas, the connection is loose, so it is here that it easily exfoliates from its pigment epithelium.
Almost throughout the optical part of the retina consists of 10 layers (see Fig. 15.1). Its photoreceptors, facing the pigment epithelium, are represented by cones (about 7 million) and rods (100-120 million). The former are grouped in the central sections of the shell, the latter are absent in the center, and their maximum density is noted at 10-13 o from it. Further to the periphery, the number of rods gradually decreases. The main elements of the retina are in a stable position due to the vertically located supporting Muller cells and interstitial tissue. The boundary membranes of the retina (membrana limitans interna et externa) also perform a stabilizing function.
Anatomically and with ophthalmoscopy in the retina, two functionally very important areas are clearly identified - the optic disc and the yellow spot, the center of which is located at a distance of 3.5 mm from the temporal edge of the disc. As you approach the yellow spot
the structure of the retina changes significantly: first, the layer of nerve fibers disappears, then the ganglion cells, then the inner plexiform layer, the layer of internal nuclei and the outer plexiform layer. The foveola of the macula is represented only by a layer of cones, therefore it has the highest resolution (the region of central vision, which occupies ~ 1.2 ° in the space of objects).
Photoreceptor parameters. Sticks: length 0.06 mm, diameter 2 µm. The outer segments contain a pigment - rhodopsin, which absorbs part of the spectrum of electromagnetic light radiation in the range of green rays (maximum 510 nm).
Cones: length 0.035 mm, diameter 6 µm. Three different types of cones (red, green and blue) contain visual pigment with different light absorption rates. In red cones, it (iodopsin) adsorbs spectral rays with a wavelength of -565 nm, in green cones - 500 nm, in blue cones - 450 nm.
The pigments of cones and rods are "embedded" in the membranes - the disks of their outer segments - and are integral protein substances.
Rods and cones have different light sensitivities. The former function at brightness environment up to 1cd? m -2 (night, scotopic vision), the second - over 10 cd? m -2 (day, photopic vision). When the brightness ranges from 1 to 10 cd?m -2 , all photoreceptors function at a certain level (twilight, mesopic vision) 1 .
The optic nerve head is located in the nasal half of the retina (at a distance of 4 mm from the posterior pole
1 Candela (cd) - a unit of luminous intensity equivalent to the brightness of a completely black body at the solidification temperature of platinum (60 cd s 1 cm 2).
eyes). It is devoid of photoreceptors, therefore, in the field of view, according to the place of its projection, there is a blind zone.
The retina is nourished from two sources: six inner layers receive it from the central retinal artery (a branch of the eye), and the neuroepithelium from the choriocapillary layer of the choroid proper.
The branches of the central arteries and veins of the retina run in the layer of nerve fibers and partly in the layer of ganglion cells. They form a layered capillary network, which is absent only in the foveolus of the macula (see Fig. 3.10).
An important anatomical feature of the retina is that the axons of its ganglion cells are devoid of myelin sheath throughout (one of the factors that determine tissue transparency). In addition, it, like the choroid, is devoid of sensitive nerve endings (see Chapter 15).
3.1.4. Inner core (cavity) of the eye
The cavity of the eye contains light-conducting and light-refracting media: aqueous humor that fills its anterior and posterior chambers, the lens and the vitreous body.
Anterior chamber of the eye(camera anterior bulbi) is a space bounded by the posterior surface of the cornea, the anterior surface of the iris and the central part of the anterior lens capsule. The place where the cornea passes into the sclera, and the iris into the ciliary body, is called the angle of the anterior chamber (angulus iridocornealis). In its outer wall there is a drainage (for aqueous humor) system of the eye, consisting of a trabecular meshwork, scleral venous sinus (Schlemm's canal) and collector tubules (graduates). Through
the pupil of the anterior chamber communicates freely with the posterior chamber. In this place, it has the greatest depth (2.75-3.5 mm), which then gradually decreases towards the periphery (see Fig. 3.2).
Posterior chamber of the eye(camera posterior bulbi) is located behind the iris, which is its anterior wall, and is bounded from the outside by the ciliary body, behind the vitreous body. The equator of the lens forms the inner wall. The entire space of the posterior chamber is permeated with ligaments of the ciliary girdle.
Normally, both chambers of the eye are filled with aqueous humor, which in its composition resembles blood plasma dialysate. The aqueous humor contains nutrients, in particular glucose, ascorbic acid and oxygen consumed by the lens and cornea, and removes waste products of metabolism from the eye - lactic acid, carbon dioxide, exfoliated pigment and other cells.
Both chambers of the eye contain 1.23-1.32 cm 3 of fluid, which is 4% of the total contents of the eye. The minute volume of chamber moisture is on average 2 mm 3 , the daily volume is 2.9 cm 3 . In other words, the complete exchange of chamber moisture occurs during
10 o'clock
Between the inflow and outflow of intraocular fluid there is an equilibrium balance. If for some reason it is violated, this leads to a change in the level of intraocular pressure, the upper limit of which normally does not exceed 27 mm Hg. Art. (when measured with a Maklakov tonometer weighing 10 g).
The main driving force that ensures a continuous flow of fluid from the posterior chamber to the anterior chamber, and then through the angle of the anterior chamber outside the eye, is the pressure difference in the eye cavity and the venous sinus of the sclera (about 10 mm Hg), as well as in the indicated sinus and anterior ciliary veins.
lens(lens) is a transparent semi-solid avascular body in the form of a biconvex lens enclosed in a transparent capsule, 9-10 mm in diameter and 3.6-5 mm thick (depending on accommodation). The radius of curvature of its anterior surface at rest of accommodation is 10 mm, the posterior surface is 6 mm (with maximum voltage accommodation 5.33 and 5.33 mm, respectively), therefore, in the first case, the refractive power of the lens is on average 19.11 diopters, in the second - 33.06 diopters. In newborns, the lens is almost spherical, has a soft texture and a refractive power of up to 35.0 diopters.
In the eye, the lens is located immediately behind the iris in a recess on the anterior surface of the vitreous body - in the vitreous fossa (fossa hyaloidea). In this position, it is held by numerous vitreous fibers, which together form a suspension ligament (ciliary girdle) (see Fig.
12.1).
The posterior surface of the lens, as well as the anterior one, is washed by aqueous humor, since it is almost completely separated from the vitreous body by a narrow slit (retrolental space - spatium retrolentale). However, along the outer edge of the vitreous fossa, this space is limited by the delicate annular ligament of Viger, located between the lens and the vitreous body. The lens is nourished by metabolic processes with chamber moisture.
vitreous chamber of the eye(camera vitrea bulbi) occupies the posterior part of its cavity and is filled with a vitreous body (corpus vitreum), which is adjacent to the lens in front, forming a small depression in this place (fossa hyaloidea), and in the rest of the length it contacts with the retina. Vitreous
the body is a transparent gelatinous mass (gel type) with a volume of 3.5-4 ml and a mass of approximately 4 g. It contains a large amount of hyaluronic acid and water (up to 98%). However, only 10% of water is associated with the components of the vitreous body, so the fluid exchange in it is quite active and, according to some sources, reaches 250 ml per day.
Macroscopically, the vitreous stroma proper (stroma vitreum) is isolated, which is pierced by the vitreous (cloquet) canal, and the hyaloid membrane surrounding it from the outside (Fig. 3.3).
The vitreous stroma consists of a fairly loose central substance, which contains optically empty zones filled with liquid (humor vitreus) and collagen fibrils. The latter, condensing, form several vitreal tracts and a denser cortical layer.
The hyaloid membrane consists of two parts - anterior and posterior. The border between them runs along the dentate line of the retina. In turn, the anterior limiting membrane has two anatomically separate parts - the lens and the zonular. The boundary between them is the circular hyaloid capsular ligament of Viger, which is strong only in childhood.
The vitreous body is tightly connected with the retina only in the region of its so-called anterior and posterior bases. The first is the area where the vitreous body is simultaneously attached to the epithelium of the ciliary body at a distance of 1-2 mm anterior to the serrated edge (ora serrata) of the retina and for 2-3 mm posterior to it. The posterior base of the vitreous body is the zone of its fixation around the optic disc. It is believed that the vitreous has a connection with the retina also in the macula.

Rice. 3.3. The vitreous body of the human eye (sagittal section) [according to N. S. Jaffe, 1969].
The vitreous (cloquet) canal (canalis hyaloideus) of the vitreous begins as a funnel-shaped extension from the edges of the optic nerve head and passes through its stroma towards the posterior lens capsule. Maximum Width channel 1-2 mm. In the embryonic period, the artery of the vitreous body passes through it, which becomes empty by the time the child is born.
As already noted, in the vitreous body there is a constant flow of fluid. From the posterior chamber of the eye, the fluid produced by the ciliary body enters the anterior vitreous through the zonular fissure. Further, the fluid that has entered the vitreous body moves to the retina and the prepapillary opening in the hyaloid membrane and flows out of the eye both through the structures of the optic nerve and along the perivascular passages.
wanderings of retinal vessels (see chapter 13).
3.1.5. Visual pathway and pupillary reflex pathway
The anatomical structure of the visual pathway is quite complex and includes a number of neural links. Within the retina of each eye is a layer of rods and cones (photoreceptors - neuron I), then a layer of bipolar (II neuron) and ganglion cells with their long axons (III neuron). Together they form the peripheral part of the visual analyzer. The pathways are represented by the optic nerves, chiasma, and optic tracts. The latter terminate in the cells of the lateral geniculate body, which plays the role of the primary visual center. The fibers of the central

Rice. 3.4. Visual and pupillary pathways (scheme) [according to C. Behr, 1931, with changes].
Explanation in the text.
visual pathway neuron (radiatio optica), which reach the area striata of the occipital lobe of the brain. Here the primary cortex is localized.
the tical center of the visual analyzer (Fig. 3.4).
optic nerve(n. opticus) formed by axons of ganglion cells
retina and ends at the chiasm. In adults, its total length varies from 35 to 55 mm. A significant part of the nerve is the orbital segment (25-30 mm), which in the horizontal plane has an S-shaped bend, due to which it does not experience tension during movements of the eyeball.
Over a considerable distance (from the exit from the eyeball to the entrance to the optic canal - canalis opticus), the nerve, like the brain, has three shells: hard, arachnoid and soft (see Fig. 3.9). Together with them, its thickness is 4-4.5 mm, without them - 3-3.5 mm. In the eyeball, the dura mater fuses with the sclera and Tenon's capsule, and in the optic canal, with the periosteum. The intracranial segment of the nerve and chiasm, located in the subarachnoid chiasmatic cistern, are dressed only in a soft shell.
The intrathecal spaces of the ophthalmic part of the nerve (subdural and subarachnoid) connect with similar spaces in the brain, but are isolated from each other. They are filled with a liquid of complex composition (intraocular, tissue, cerebrospinal). Because the intraocular pressure normally 2 times higher than intracranial (10-12 mm Hg), the direction of its current coincides with the pressure gradient. The exception is cases when intracranial pressure is significantly increased (for example, with the development of a brain tumor, hemorrhages in the cranial cavity) or, conversely, the tone of the eye is significantly reduced.
All nerve fibers that make up the optic nerve are grouped into three main bundles. Axons of ganglion cells extending from the central (macular) region of the retina make up the papillomacular bundle, which enters the temporal half of the optic nerve head. Fibers from ganglionic
cells of the nasal half of the retina go along radial lines into the nasal half of the disc. Similar fibers, but from the temporal half of the retina, on the way to the optic nerve head, “flow around” the papillomacular bundle from above and below.
In the orbital segment of the optic nerve near the eyeball, the ratios between the nerve fibers remain the same as in its disk. Next, the papillomacular bundle moves to the axial position, and the fibers from the temporal quadrants of the retina - to the entire corresponding half of the optic nerve. Thus, the optic nerve is clearly divided into right and left halves. Its division into upper and lower halves is less pronounced. An important clinical feature is that the nerve is devoid of sensitive nerve endings.
In the cranial cavity, the optic nerves connect over the area of the Turkish saddle, forming chiasma (chiasma opticum), which is covered with a pia mater and has the following dimensions: length 4-10 mm, width 9-11 mm, thickness 5 mm. Chiasma from below borders on the diaphragm of the Turkish saddle (a preserved section of the dura mater), from above (in the posterior section) - to the bottom of the third ventricle of the brain, on the sides - to the internal carotid arteries, behind - to the pituitary funnel.
In the region of the chiasm, the fibers of the optic nerves partially cross due to portions associated with the nasal halves of the retinas. Moving to the opposite side, they connect with fibers coming from the temporal halves of the retinas of the other eye, and form the visual tracts. Here, the papillomacular bundles also partially intersect.
The optic tracts (tractus opticus) begin at the posterior surface of the chiasm and, rounding from the outer
sides of the brain stem, terminate in the external geniculate body (corpus geniculatum laterale), the back of the visual tubercle (thalamus opticus) and the anterior quadrigemina (corpus quadrigeminum anterius) of the corresponding side. However, only the external geniculate bodies are the unconditional subcortical visual center. The remaining two formations perform other functions.
In the visual tracts, whose length in an adult reaches 30-40 mm, the papillomacular bundle also occupies a central position, and the crossed and non-crossed fibers still go in separate bundles. At the same time, the first of them are located ventromedially, and the second - dorsolaterally.
Visual radiation (fibers of the central neuron) starts from the ganglion cells of the fifth and sixth layers of the lateral geniculate body. First, the axons of these cells form the so-called Wernicke's field, and then, passing through the posterior thigh of the internal capsule, fan-shaped diverge in the white matter of the occipital lobe of the brain. The central neuron ends in the furrow of the bird's spur (sulcus calcarinus). This area personifies the sensory visual center - the cortical field 17 according to Brodmann.
The path of the pupillary reflex - light and to set the eyes at a close distance - is rather complicated (see Fig. 3.4). The afferent part of the reflex arc (a) of the first of them starts from the cones and rods of the retina in the form of autonomous fibers that go as part of the optic nerve. In the chiasm, they cross in exactly the same way as the optic fibers and pass into the optic tracts. In front of the external geniculate bodies, the pupillomotor fibers leave them and, after a partial decussation, continue into the brachium quadrigeminum, where
end at the cells (b) of the so-called pretectal area (area pretectalis). Further, new, interstitial neurons, after partial decussation, are sent to the corresponding nuclei (Yakubovich - Edinger - Westphal) of the oculomotor nerve (c). Afferent fibers from the macula lutea of each eye are present in both oculomotor nuclei (d).
The efferent path of innervation of the iris sphincter starts from the already mentioned nuclei and goes as a separate bundle as part of the oculomotor nerve (n. oculomotorius) (e). In the orbit, the sphincter fibers enter its lower branch, and then through the oculomotor root (radix oculomotoria) into the ciliary node (e). Here the first neuron of the path under consideration ends and the second one begins. Upon exiting the ciliary node, the sphincter fibers in the composition of the short ciliary nerves (nn. ciliares breves), passing through the sclera, enter the perichoroidal space, where they form the nerve plexus (g). Its terminal branches penetrate the iris and enter the muscle in separate radial bundles, that is, they innervate it sectorally. In total, there are 70-80 such segments in the sphincter of the pupil.
The efferent path of the pupil dilator (m. dilatator pupillae), which receives sympathetic innervation, starts from the ciliospinal center Budge. The latter is located in the anterior horns of the spinal cord (h) between C VII and Th II. Connecting branches depart from here, which through the border trunk of the sympathetic nerve (l), and then the lower and middle sympathetic cervical ganglia (t 1 and t 2) reach the upper ganglion (t 3) (level C II - C IV). Here the first neuron of the path ends and the second begins, which is part of the plexus of the internal carotid artery (m). In the cranial cavity, the fibers innervating the dilat-
torus of the pupil, exit from the mentioned plexus, enter the trigeminal (Gasser) node (gangl. trigeminal), and then leave it as part of the ophthalmic nerve (n. ophthalmicus). Already at the top of the orbit, they pass into the nasociliary nerve (n. nasociliaris) and then, together with the long ciliary nerves (nn. ciliares longi), penetrate into the eyeball 1.
The pupillary dilator function is regulated by the supranuclear hypothalamic center, located at the level of the bottom of the third ventricle of the brain in front of the pituitary infundibulum. Through the reticular formation, it is connected with the ciliospinal center Budge.
The reaction of the pupils to convergence and accommodation has its own characteristics, and the reflex arcs in this case differ from those described above.
With convergence, the stimulus for pupillary constriction is proprioceptive impulses coming from the contracting internal rectus muscles of the eye. Accommodation is stimulated by the vagueness (defocusing) of images of external objects on the retina. The efferent part of the pupillary reflex arc is the same in both cases.
The center for setting the eye at close range is believed to be in Brodmann's cortical area 18.
3.2. The eye socket and its contents
The orbit (orbita) is the bony receptacle for the eyeball. Through its cavity, the posterior (retrobulbar) section of which is filled with a fatty body (corpus adiposum orbitae), the optic nerve, motor and sensory nerves, oculomotor muscles pass through it.
1 In addition, the central sympathetic pathway (s) departs from the Budge center, ending in the cortex of the occipital lobe of the brain. From here begins the corticonuclear pathway of inhibition of the pupillary sphincter.
tsy, muscle that lifts the upper eyelid, fascial formations, blood vessels. Each eye socket has the shape of a truncated tetrahedral pyramid with its apex facing the skull at an angle of 45 o to the sagittal plane. In an adult, the depth of the orbit is 4-5 cm, the horizontal diameter at the entrance (aditus orbitae) is about 4 cm, and the vertical diameter is 3.5 cm (Fig. 3.5). Three of the four walls of the orbit (except the outer one) border on the paranasal sinuses. This neighborhood often serves as the initial cause of the development of certain pathological processes in it, more often of an inflammatory nature. Germination of tumors emanating from the ethmoid, frontal and maxillary sinuses is also possible (see Chapter 19).
The outer, most durable and least vulnerable to diseases and injuries, the wall of the orbit is formed by the zygomatic, partly frontal bone and a large wing of the sphenoid bone. This wall separates the contents of the orbit from the temporal fossa.
The upper wall of the orbit is formed mainly by the frontal bone, in the thickness of which, as a rule, there is a sinus (sinus frontalis), and partly (in the posterior section) by the small wing of the sphenoid bone; borders on the anterior cranial fossa, and this circumstance determines the severity possible complications when it is damaged. On the inner surface of the orbital part of the frontal bone, at its lower edge, there is a small bony protrusion (spina trochlearis), to which the tendon loop is attached. The tendon of the superior oblique muscle passes through it, which then abruptly changes the direction of its course. In the upper outer part of the frontal bone there is a fossa of the lacrimal gland (fossa glandulae lacrimalis).
The inner wall of the orbit over a large extent is formed by a very thin bone plate - lam. orbitalis (rarugasea) re-

Rice. 3.5. Eye socket (right).
ethmoid bone. In front, the lacrimal bone with the posterior lacrimal crest and the frontal process of the upper jaw with the anterior lacrimal crest adjoin it, behind it is the body of the sphenoid bone, above it is part of the frontal bone, and below is part of the upper jaw and palatine bone. Between the crests of the lacrimal bone and the frontal process of the upper jaw there is a recess - the lacrimal fossa (fossa sacci lacrimalis) measuring 7 x 13 mm, in which the lacrimal sac (saccus lacrimalis) is located. Below, this fossa passes into the nasolacrimal canal (canalis nasolacrimalis), located in the wall of the maxillary bone. It contains the nasolacrimal duct (ductus nasolacrimalis), which ends at a distance of 1.5-2 cm posterior to the anterior edge of the inferior turbinate. Due to its fragility, the medial wall of the orbit is easily damaged even with blunt trauma with the development of emphysema of the eyelids (more often) and the orbit itself (less often). In addition, patho-
the logical processes that occur in the ethmoid sinus spread quite freely towards the orbit, resulting in the development of inflammatory edema of its soft tissues (cellulitis), phlegmon or optic neuritis.
The lower wall of the orbit is also the upper wall of the maxillary sinus. This wall is formed mainly by the orbital surface of the upper jaw, partly also by the zygomatic bone and the orbital process of the palatine bone. With injuries, fractures of the lower wall are possible, which are sometimes accompanied by omission of the eyeball and limitation of its mobility upward and outward when the inferior oblique muscle is infringed. The lower wall of the orbit begins from the bone wall, slightly lateral to the entrance to the nasolacrimal canal. Inflammatory and tumor processes that develop in the maxillary sinus spread quite easily towards the orbit.
At the top in the walls of the orbit there are several holes and crevices through which a number of large nerves and blood vessels pass into its cavity.
1. Bone canal of the optic nerve (canalis opticus) 5-6 mm long. It begins in the orbit with a round hole (foramen opticum) with a diameter of about 4 mm, connects its cavity with the middle cranial fossa. Through this canal, the optic nerve (n. opticus) and the ophthalmic artery (a. ophthalmica) enter the orbit.
2. Upper orbital fissure (fissura orbitalis superior). Formed by the body of the sphenoid bone and its wings, connects the orbit with the middle cranial fossa. Tightened with a thin connective tissue film, through which three main branches of the ophthalmic nerve pass into the orbit (n. ophthalmicus 1 - lacrimal, nasociliaris and frontal nerves (nn. lacrimalis, nasociliaris et frontalis), as well as the trunks of the block, abducent and oculomotor nerves (nn. trochlearis, abducens and oculomotorius).The superior ophthalmic vein (v. ophthalmica superior) leaves it through the same gap. In case of damage to this area, a characteristic symptom complex develops: complete ophthalmoplegia, that is, immobility of the eyeball, drooping (ptosis) of the upper eyelid, mydriasis, decrease tactile sensitivity cornea and eyelid skin, retinal vein dilatation and slight exophthalmos. However, the "syndrome of the superior orbital fissure" may not be fully expressed when not all are damaged, but only individual nerve trunks passing through this fissure.
3. Lower orbital fissure (fissura orbitalis inferior). Formed by the lower edge of the large wing of the sphenoid bone and the body of the upper jaw, provides communication
1 First branch trigeminal nerve(n. trigeminus).
orbits with pterygopalatine (in the posterior half) and temporal fossae. This gap is also closed by a connective tissue membrane, into which the fibers of the orbital muscle (m. Orbitalis), innervated by the sympathetic nerve, are woven. Through it, one of the two branches of the inferior ophthalmic vein leaves the orbit (the other flows into the superior ophthalmic vein), which then anastomoses with the pterygoid venous plexus (et plexus venosus pterygoideus), and the infraorbital nerve and artery (n. a. infraorbital), zygomatic nerve (n. zygomaticus) enter ) and orbital branches of the pterygopalatine ganglion (ganglion pterygopalatinum).
4. A round hole (foramen rotundum) is located in the large wing of the sphenoid bone. It connects the middle cranial fossa with the pterygopalatine. The second branch of the trigeminal nerve (n. maxillaris) passes through this hole, from which the infraorbital nerve (n. infraorbitalis) departs in the pterygopalatine fossa, and the zygomatic nerve (n. zygomaticus) in the inferior temporal fossa. Both nerves then enter the orbital cavity (the first is subperiosteal) through the inferior orbital fissure.
5. Lattice holes on the medial wall of the orbit (foramen ethmoidale anterius et posterius), through which the nerves of the same name (branches of the nasociliary nerve), arteries and veins pass.
In addition, in the large wing of the sphenoid bone there is another hole - oval (foramen ovale), connecting the middle cranial fossa with the infratemporal. The third branch of the trigeminal nerve (n. mandibularis) passes through it, but it does not take part in the innervation of the organ of vision.
Behind the eyeball, at a distance of 18-20 mm from its posterior pole, there is a ciliary ganglion (ganglion ciliare) 2x1 mm in size. It is located under the external rectus muscle, adjoining in this zone to the
top of the optic nerve. The ciliary ganglion is a peripheral nerve ganglion, the cells of which, through three roots (radix nasociliaris, oculomotoria et sympathicus), are connected to the fibers of the corresponding nerves.
The bony walls of the orbit are covered with a thin but strong periosteum (periorbita), which is tightly fused with them in the area of the bone sutures and the optic canal. The opening of the latter is surrounded by a tendon ring (annulus tendineus communis Zinni), from which all the oculomotor muscles originate, with the exception of the inferior oblique. It originates from the lower bone wall of the orbit, near the inlet of the nasolacrimal canal.
In addition to the periosteum, the fasciae of the orbit, according to the International Anatomical Nomenclature, include the vagina of the eyeball, muscular fascia, the orbital septum, and the fatty body of the orbit (corpus adiposum orbitae).
The vagina of the eyeball (vagina bulbi, the former name is fascia bulbi s. Tenoni) covers almost the entire eyeball, with the exception of the cornea and the exit point of the optic nerve. The greatest density and thickness of this fascia are noted in the region of the equator of the eye, where the tendons of the oculomotor muscles pass through it on the way to the places of attachment to the surface of the sclera. As it approaches the limbus, the vaginal tissue becomes thinner and eventually is gradually lost in the subconjunctival tissue. In places of cutting by extraocular muscles, it gives them a fairly dense connective tissue coating. Dense strands (fasciae musculares) also depart from this zone, connecting the vagina of the eye with the periosteum of the walls and edges of the orbit. In general, these strands form an annular membrane that is parallel to the equator of the eye.
and keeps it in the eye socket in a stable position.
The subvaginal space of the eye (formerly called spatium Tenoni) is a system of slits in loose episcleral tissue. It provides free movement of the eyeball in a certain volume. This space is often used for surgical and therapeutic purposes (performing implant-type sclero-strengthening operations, administering drugs by injection).
The orbital septum (septum orbitale) is a well-defined fascial-type structure located in the frontal plane. Connects the orbital edges of the cartilages of the eyelids with the bony edges of the orbit. Together they form, as it were, its fifth, mobile wall, which, with closed eyelids, completely isolates the cavity of the orbit. It is important to keep in mind that in the region of the medial wall of the orbit, this septum, which is also called the tarsoorbital fascia, is attached to the posterior lacrimal crest of the lacrimal bone, as a result of which the lacrimal sac, which lies closer to the surface, is partially located in the preseptal space, i.e., outside the cavity eye sockets.
The cavity of the orbit is filled with a fatty body (corpus adiposum orbitae), which is enclosed in a thin aponeurosis and permeated with connective tissue bridges that divide it into small segments. Due to its plasticity, adipose tissue does not interfere with the free movement of the oculomotor muscles passing through it (during their contraction) and the optic nerve (during movements of the eyeball). The fat body is separated from the periosteum by a slit-like space.
Through the orbit in the direction from its top to the entrance pass various blood vessels, motor, sensory and sympathetic.
tic nerves, which has already been partially mentioned above, and is detailed in the corresponding section of this chapter. The same applies to the optic nerve.
3.3. Accessory organs of the eye
The auxiliary organs of the eye (organa oculi accesoria) include the eyelids, the conjunctiva, the muscles of the eyeball, the lacrimal apparatus, and the orbital fascia already described above.
3.3.1. Eyelids
Eyelids (palpebrae), upper and lower, - mobile structural formations covering the front of the eyeballs (Fig. 3.6). Thanks to blinking movements, they contribute to a uniform distribution of tear fluid over their surface. The upper and lower eyelids at the medial and lateral angles are interconnected by means of adhesions (comissura palpebralis medialis et lateralis). Approximately for

Rice. 3.6. Eyelids and anterior segment of the eyeball (sagittal section).
5 mm before confluence, the inner edges of the eyelids change the direction of their course and form an arcuate bend. The space outlined by them is called the lacrimal lake (lacus lacrimalis). There is also a small pinkish elevation - the lacrimal caruncle (caruncula lacrimalis) and the adjacent semilunar fold of the conjunctiva (plica semilunaris conjunctivae).
With open eyelids, their edges limit an almond-shaped space called the palpebral fissure (rima palpebrarum). Its horizontal length is 30 mm (in an adult), and the height in the central section ranges from 10 to 14 mm. Within the palpebral fissure, almost the entire cornea is visible, with the exception of the upper segment, and the white sclera bordering it. With closed eyelids, the palpebral fissure disappears.
Each eyelid consists of two plates: outer (musculocutaneous) and inner (tarsal-conjunctival).
The skin of the eyelids is delicate, easily folded and supplied with sebaceous and sweat glands. The fiber lying under it is devoid of fat and very loose, which contributes to the rapid spread of edema and hemorrhage in this place. Usually, two orbital-palpebral folds are clearly visible on the skin surface - upper and lower. As a rule, they coincide with the corresponding edges of the cartilage.
The cartilages of the eyelids (tarsus superior et inferior) look like horizontal plates slightly convex outwards with rounded edges, about 20 mm long, 10-12 and 5-6 mm high, respectively, and 1 mm thick. They are made up of very dense connective tissue. With the help of powerful ligaments (lig. palpebrale mediate et laterale), the ends of the cartilage are connected to the corresponding walls of the orbit. In turn, the orbital edges of the cartilage are firmly connected
us with the edges of the orbit by means of fascial tissue (septum orbitale).
In the thickness of the cartilage are oblong alveolar meibomian glands (glandulae tarsales) - about 25 in the upper cartilage and 20 in the lower. They run in parallel rows and open with excretory ducts near the posterior margin of the eyelids. These glands produce a lipid secretion that forms the outer layer of the precorneal tear film.
The posterior surface of the eyelids is covered with a connective sheath (conjunctiva), which is tightly fused with cartilage, and outside it forms mobile vaults - a deep upper and a shallower, lower one that is easily accessible for inspection.
The free edges of the eyelids are limited by the anterior and posterior ridges (limbi palpebrales anteriores et posteriores), between which there is a space about 2 mm wide. The anterior ridges carry the roots of numerous eyelashes (arranged in 2-3 rows), into the hair follicles of which the sebaceous (Zeiss) and modified sweat (Moll) glands open. On the back ridges of the lower and upper eyelids, in their medial part, there are small elevations - lacrimal papillae (papilli lacrimales). They are immersed in the lacrimal lake and are provided with pinholes (punctum lacrimale) leading to the corresponding lacrimal tubules (canaliculi lacrimales).
The mobility of the eyelids is provided by the action of two antagonistic muscle groups - closing and opening them. The first function is realized with the help of the circular muscle of the eye (m. orbicularis oculi), the second - with the muscle that lifts the upper eyelid (m. levator palpebrae superioris) and the lower tarsal muscle (m. tarsalis inferior).
The circular muscle of the eye consists of three parts: orbital (pars orbitalis), secular (pars palpebralis) and lacrimal (pars lacrimalis) (Fig. 3.7).

Rice. 3.7. Circular muscle of the eye.
The orbital part of the muscle is a circular pulp, the fibers of which begin and attach at the medial ligament of the eyelids (lig. palpebrale mediale) and the frontal process of the upper jaw. Contraction of the muscle leads to a tight closure of the eyelids.
The fibers of the secular part of the circular muscle also start from the medial ligament of the eyelids. Then the course of these fibers becomes arcuate and they reach the outer canthus, where they are attached to the lateral ligament of the eyelids (lig. palpebrale laterale). The contraction of this group of fibers ensures the closure of the eyelids and their blinking movements.
The lacrimal part of the orbicular muscle of the eyelid is represented by a deeply located portion of muscle fibers that begin somewhat posteriorly from the posterior lacrimal crest of the lacrimal bone. Then they pass behind the lacrimal sac and are woven into the fibers of the secular part of the circular muscle, coming from the anterior lacrimal crest. As a result, the lacrimal sac is covered by a muscle loop, which, during contractions and relaxation during
the time of blinking movements of the eyelids either expands or narrows the lumen of the lacrimal sac. Due to this, the lacrimal fluid is absorbed from the conjunctival cavity (through the lacrimal openings) and moves along the lacrimal ducts into the nasal cavity. This process is also facilitated by contractions of those bundles of the lacrimal muscle that surround the lacrimal canaliculi.
Particularly distinguished are those muscle fibers of the circular muscle of the eyelid, which are located between the roots of the eyelashes around the ducts of the meibomian glands (m. ciliaris Riolani). The contraction of these fibers contributes to the secretion of the mentioned glands and the pressing of the edges of the eyelids to the eyeball.
The circular muscle of the eye is innervated by the zygomatic and anterior temporal branches of the facial nerve, which lie deep enough and enter it mainly from the lower outer side. This circumstance should be taken into account if it is necessary to produce muscle akinesia (usually when performing abdominal operations on the eyeball).
The muscle that lifts the upper eyelid begins near the optic canal, then goes under the roof of the orbit and ends in three portions - superficial, medium and deep. The first of them, turning into a wide aponeurosis, passes through the orbital septum, between the fibers of the secular part of the circular muscle and ends under the skin of the eyelid. The middle portion, consisting of a thin layer of smooth fibers (m. tarsalis superior, m. Mülleri), is woven into the upper edge of the cartilage. The deep plate, like the superficial one, also ends with a tendon stretch, which reaches the upper fornix of the conjunctiva and is attached to it. Two portions of the levator (superficial and deep) are innervated by the oculomotor nerve, the middle one by the cervical sympathetic nerve.
The lower eyelid is pulled down by a poorly developed eye muscle (m. tarsalis inferior), which connects the cartilage with the lower fornix of the conjunctiva. Special processes of the sheath of the lower rectus muscle are also woven into the latter.
The eyelids are richly supplied with vessels due to the branches of the ophthalmic artery (a. ophthalmica), which is part of the system of the internal carotid artery, as well as anastomoses from the facial and maxillary arteries (a. facialis et maxillaris). The last two arteries already belong to the external carotid artery. Branching, all these vessels form arterial arches - two on the upper eyelid and one on the lower.
The eyelids also have a well-developed lymphatic network, which is located on two levels - on the anterior and posterior surfaces of the cartilage. In this case, the lymphatic vessels of the upper eyelid flow into the anterior lymph nodes, and the lower - into the submandibular.
Sensitive innervation of the skin of the face is carried out by three branches of the trigeminal nerve and branches of the facial nerve (see Chapter 7).
3.3.2. Conjunctiva
Conjunctiva (tunica conjunctiva) - a thin (0.05-0.1 mm) mucous membrane that covers the entire back surface of the eyelids (tunica conjunctiva palpebrarum), and then, having formed the arches of the conjunctival sac (fornix conjunctivae superior et inferior), passes to the anterior the surface of the eyeball (tunica conjunctiva bulbi) and ends at the limbus (see Fig. 3.6). It is called the connective sheath, as it connects the eyelid and eye.
In the conjunctiva of the eyelids, two parts are distinguished - the tarsal, tightly fused with the underlying tissue, and the mobile orbital in the form of a transitional (to the vaults) fold.
When the eyelids are closed, a slit-like cavity is formed between the sheets of the conjunctiva, deeper at the top, resembling a bag. When the eyelids are open, its volume decreases markedly (by the size of the palpebral fissure). The volume and configuration of the conjunctival sac also change significantly with eye movements.
The cartilage conjunctiva is covered with stratified columnar epithelium and contains goblet cells at the edge of the eyelids, and the crypts of Henle near the distal end of the cartilage. Both those and others secrete mucin. Normally, the meibomian glands are visible through the conjunctiva, forming a pattern in the form of a vertical palisade. Under the epithelium is reticular tissue, firmly soldered to the cartilage. At the free edge of the eyelid, the conjunctiva is smooth, but already at a distance of 2-3 mm from it it becomes rough due to the presence of papillae here.
The conjunctiva of the transitional fold is smooth and covered with a 5-6-layered squamous epithelium with a large number of goblet mucous cells (mucin is secreted). Its subepithelial loose connective tissue
This tissue, consisting of elastic fibers, contains plasma cells and lymphocytes that can form clusters in the form of follicles or lymphomas. Due to the presence of well-developed subconjunctival tissue, this part of the conjunctiva is very mobile.
On the border between the tarsal and orbital parts of the conjunctiva there are additional lacrimal glands of Wolfring (3 at the upper edge of the upper cartilage and one more below the lower cartilage), and in the area of the arches - Krause's glands, the number of which is 6-8 in the lower eyelid and 15-40 - on the top. In structure, they are similar to the main lacrimal gland, the excretory ducts of which open in the lateral part of the superior conjunctival fornix.
The conjunctiva of the eyeball is covered with stratified squamous non-keratinized epithelium and is loosely connected to the sclera, so it can easily move along its surface. The limbal part of the conjunctiva contains islands of columnar epithelium with secreting Becher cells. In the same zone, radially to the limbus (in the form of a belt 1-1.5 mm wide), there are Mantz cells that produce mucin.
The blood supply of the conjunctiva of the eyelids is carried out at the expense of the vascular trunks extending from the arterial arches of the palpebral arteries (see Fig. 3.13). The conjunctiva of the eyeball contains two layers of blood vessels - superficial and deep. The superficial is formed by branches extending from the arteries of the eyelids, as well as the anterior ciliary arteries (branches of the muscular arteries). The first of them go in the direction from the arches of the conjunctiva to the cornea, the second - towards them. The deep (episcleral) vessels of the conjunctiva are branches of only the anterior ciliary arteries. They are directed towards the cornea and form a dense network around it. Os-
the new trunks of the anterior ciliary arteries, before reaching the limbus, go inside the eye and participate in the blood supply to the ciliary body.
The veins of the conjunctiva accompany the corresponding arteries. The outflow of blood goes mainly through the palpebral system of vessels into the facial veins. The conjunctiva also has a rich network of lymphatic vessels. The outflow of lymph from the mucous membrane of the upper eyelid occurs in the anterior lymph nodes, and from the lower - in the submandibular.
Sensitive innervation of the conjunctiva is provided by the lacrimal, subtrochlear and infraorbital nerves (nn. lacrimalis, infratrochlearis et n. infraorbitalis) (see Chapter 9).
3.3.3. Muscles of the eyeball
The muscular apparatus of each eye (musculus bulbi) consists of three pairs of antagonistically acting oculomotor muscles: upper and lower rectus (mm. rectus oculi superior et inferior), internal and outer rectus (mm. rectus oculi medialis et lataralis), superior and inferior oblique ( mm. obliquus superior et inferior) (see chapter 18 and fig. 18.1).
All muscles, with the exception of the inferior oblique, begin, like the muscle that lifts the upper eyelid, from the tendon ring located around the optic canal of the orbit. Then the four rectus muscles are directed, gradually diverging, anteriorly, and after perforation of the Tenon's capsule, they are woven with their tendons into the sclera. The lines of their attachment are at different distances from the limbus: the inner straight line - 5.5-5.75 mm, the lower one - 6-6.5 mm, the outer one 6.9-7 mm, the upper one - 7.7-8 mm.
The superior oblique muscle from the optic opening goes to the bone-tendon block located at the upper inner corner of the orbit and, having spread over
him, goes backwards and outwards in the form of a compact tendon; attached to the sclera in the upper outer quadrant of the eyeball at a distance of 16 mm from the limbus.
The inferior oblique muscle starts from the inferior bone wall of the orbit somewhat lateral to the entrance to the nasolacrimal canal, goes posteriorly and outwardly between the inferior wall of the orbit and the inferior rectus muscle; attached to the sclera at a distance of 16 mm from the limbus (inferior outer quadrant of the eyeball).
The internal, superior and inferior rectus muscles, as well as the inferior oblique muscle, are innervated by branches of the oculomotor nerve (n. oculomotorius), the external rectus - the abducens (n. abducens), the superior oblique - block (n. trochlearis).
When a particular muscle of the eye contracts, it moves around an axis that is perpendicular to its plane. The latter runs along the muscle fibers and crosses the point of rotation of the eye. This means that in most oculomotor muscles (with the exception of the external and internal rectus muscles) the axes of rotation have one or another angle of inclination with respect to the initial coordinate axes. As a result, when such muscles contract, the eyeball makes a complex movement. So, for example, the superior rectus muscle, in the middle position of the eye, lifts it up, rotates inwards and turns somewhat towards the nose. It is clear that the amplitude of vertical eye movements will increase as the angle of divergence between the sagittal and muscular planes decreases, i.e., when the eye is turned outward.
All movements of the eyeballs are divided into combined (associated, conjugated) and convergent (fixation of objects at different distances due to convergence). Combined movements are those that are directed in one direction:
up, right, left, etc. These movements are performed by synergistic muscles. So, for example, when looking to the right, the external rectus muscle contracts in the right eye, and the internal rectus muscle in the left eye. Convergent movements are realized through the action of the internal rectus muscles of each eye. A variation of them are fusion movements. Being very small, they carry out a particularly precise fixation of the eyes, which creates conditions for unimpeded merging of two retinal images in the cortical section of the analyzer into one solid image.
3.3.4. lacrimal apparatus
The production of lacrimal fluid is carried out in the lacrimal apparatus (apparatus lacrimalis), consisting of the lacrimal gland (glandula lacrimalis) and the small accessory glands of Krause and Wolfring. The latter provide the daily requirement of the eye for its moisturizing fluid. The main lacrimal gland actively functions only in conditions of emotional outbursts (positive and negative), as well as in response to irritation of sensitive nerve endings in the mucous membrane of the eye or nose (reflex tearing).
The lacrimal gland lies under the upper outer edge of the orbit in the deepening of the frontal bone (fossa glandulae lacrimalis). The tendon of the muscle that lifts the upper eyelid divides it into a large orbital and a smaller secular part. The excretory ducts of the orbital lobe of the gland (in the amount of 3-5) pass between the lobules of the secular gland, taking along a number of its numerous small ducts, and open in the fornix of the conjunctiva at a distance of several millimeters from the upper edge of the cartilage. In addition, the secular part of the gland also has independent proto-
ki, the number of which is from 3 to 9. Since it lies immediately under the upper fornix of the conjunctiva, when the upper eyelid is everted, its lobed contours are usually clearly visible.
The lacrimal gland is innervated by the secretory fibers of the facial nerve (n. facialis), which, after a difficult path, reach it as part of the lacrimal nerve (n. lacrimalis), which is a branch of the ophthalmic nerve (n. ophthalmicus).
In children, the lacrimal gland begins to function by the end of the 2nd month of life, therefore, until this period expires, when crying, their eyes remain dry.
The lacrimal fluid produced by the glands mentioned above rolls down the surface of the eyeball from top to bottom into the capillary gap between the posterior crest of the lower eyelid and the eyeball, where a lacrimal stream (rivus lacrimalis) is formed, which flows into the lacrimal lake (lacus lacrimalis). The blinking movements of the eyelids contribute to the promotion of tear fluid. When closing, they not only go towards each other, but also move inwards (especially the lower eyelid) by 1-2 mm, as a result of which the palpebral fissure is shortened.
The lacrimal ducts consist of the lacrimal ducts, the lacrimal sac, and the nasolacrimal duct (see Chapter 8 and Figure 8.1).
Lacrimal tubules (canaliculi lacrimales) begin with lacrimal punctures (punctum lacrimale), which are located on top of the lacrimal papillae of both eyelids and are immersed in the lacrimal lake. The diameter of the dots with open eyelids is 0.25-0.5 mm. They lead to the vertical part of the tubules (length 1.5-2 mm). Then their course changes to almost horizontal. Then, gradually approaching, they open into the lacrimal sac behind the internal commissure of the eyelids, each individually or having previously merged into a common mouth. The length of this part of the tubules is 7-9 mm, the diameter
0.6 mm. The walls of the tubules are covered with stratified squamous epithelium, under which there is a layer of elastic muscle fibers.
The lacrimal sac (saccus lacrimalis) is located in a vertically elongated bone fossa between the anterior and posterior knees of the internal commissure of the eyelids and is covered by a muscular loop (m. Horneri). Its dome protrudes above this ligament and is located preseptally, that is, outside the cavity of the orbit. From the inside, the bag is covered with stratified squamous epithelium, under which there is a layer of adenoid, and then dense fibrous tissue.
The lacrimal sac opens into the nasolacrimal duct (ductus nasolacrimalis), which first passes through the bone canal (about 12 mm long). In the lower section, it has a bone wall only on the lateral side, in other sections it borders on the nasal mucosa and is surrounded by a dense venous plexus. The duct opens under the inferior nasal concha at a distance of 3-3.5 cm from the external opening of the nose. Its total length is 15 mm, diameter is 2-3 mm. In newborns, the outlet of the duct is often closed with a mucous plug or a thin film, as a result of which conditions are created for the development of purulent or serous-purulent dacryocystitis. The wall of the duct has the same structure as the wall of the lacrimal sac. At the outlet of the duct, the mucous membrane forms a fold, which plays the role of a closing valve.
In general, it can be assumed that the lacrimal duct consists of small soft tubes of various lengths and shapes with a changing diameter, which are joined under certain angles. They connect the conjunctival cavity with the nasal cavity, where there is a constant outflow of tear fluid. It is provided by blinking movements of the eyelids, a siphon effect with capillary
the tension of the fluid filling the lacrimal ducts, the peristaltic change in the diameter of the tubules, the suction ability of the lacrimal sac (due to the alternation of positive and negative pressure in it when blinking) and the negative pressure created in the nasal cavity during the aspiration of air.
3.4. Blood supply to the eye and its accessory organs
3.4.1. Arterial system of the organ of vision
The main role in the nutrition of the organ of vision is played by the ophthalmic artery (a. ophthalmica) - one of the main branches of the internal carotid artery. Through the optic canal, the ophthalmic artery enters the cavity of the orbit and, being first under the optic nerve, then rises from the outside upwards and crosses it, forming an arc. From her and from
all the main branches of the ophthalmic artery go (Fig. 3.8).
The central retinal artery (a. centralis retinae) is a vessel of small diameter, coming from the initial part of the arc of the ophthalmic artery. At a distance of 7-12 mm from the posterior pole of the eye through the hard shell, it enters from below into the depths of the optic nerve and is directed towards its disc by a single trunk, giving off a thin horizontal branch in the opposite direction (Fig. 3.9). Often, however, there are cases when the ophthalmic part of the nerve is fed by a small vascular branch, which is often called the central artery of the optic nerve (a. centralis nervi optici). Its topography is not constant: in some cases it departs into various options from the central retinal artery, in others - directly from the ophthalmic artery. In the center of the nerve trunk, this artery after a T-shaped division

Rice. 3.8. Blood vessels of the left eye socket (top view) [from the work of M. L. Krasnov, 1952, with changes].

Rice. 3.9. Blood supply to the optic nerve and retina (scheme) [according to H. Remky,
1975].
occupies a horizontal position and sends multiple capillaries towards the vasculature of the pia mater. The intratubular and peritubular parts of the optic nerve are fed by r. recurrences a. ophthalmica, r. recurrences a. hypophysial
sup. ant. and rr. intracanaliculares a. ophthalmica.
The central retinal artery emerges from the stem part of the optic nerve, dichotomously divides up to the 3rd order arterioles (Fig. 3.10), forming vascular

Rice. 3.10. Topography of the terminal branches of the central arteries and veins of the retina of the right eye in the diagram and photograph of the fundus.
a dense network that nourishes the medulla of the retina and the intraocular part of the optic nerve head. Not so rare in the fundus with ophthalmoscopy, you can see an additional power source of the macular zone of the retina in the form of a. cilioretinalis. However, it no longer departs from the ophthalmic artery, but from the posterior short ciliary or arterial circle of Zinn-Haller. Its role is very great in circulatory disorders in the system of the central retinal artery.
Posterior short ciliary arteries (aa. ciliares posteriores breves) - branches (6-12 mm long) of the ophthalmic artery that approach the sclera of the posterior pole of the eye and, perforating it around the optic nerve, form the intrascleral arterial circle of Zinn-Haller. They also form the vascular
shell - the choroid (Fig.
3.11). The latter, through its capillary plate, nourishes the neuroepithelial layer of the retina (from the layer of rods and cones to the outer plexiform inclusive). Separate branches of the posterior short ciliary arteries penetrate the ciliary body, but do not play a significant role in its nutrition. In general, the system of short posterior ciliary arteries does not anastomose with any other vascular plexuses of the eye. It is for this reason that inflammatory processes that develop in the choroid itself are not accompanied by hyperemia of the eyeball. . Two posterior long ciliary arteries (aa. ciliares posteriores longae) depart from the trunk of the ophthalmic artery and are located distally

Rice. 3.11. Blood supply to the vascular tract of the eye [according to Spalteholz, 1923].

Rice. 3.12. Vascular system of the eye [according to Spalteholz, 1923].
posterior short ciliary arteries. The sclera is perforated at the level of the lateral sides of the optic nerve and, having entered the suprachoroidal space at 3 and 9 o'clock, they reach the ciliary body, which is mainly nourished. Anastomose with the anterior ciliary arteries, which are branches of the muscular arteries (aa. musculares) (Fig. 3.12).
Near the root of the iris, the posterior long ciliary arteries divide dichotomously. The resulting branches are connected to each other and form a large arterial
circle of the iris (circulus arteriosus iridis major). New branches depart from it in the radial direction, forming, in turn, already on the border between the pupillary and ciliary zones of the iris, a small arterial circle (circulus arteriosus iridis minor).
The posterior long ciliary arteries are projected onto the sclera in the area of passage of the internal and external rectus muscles of the eye. These guidelines should be kept in mind when planning operations.
Muscular arteries (aa. musculares) are usually represented by two
more or less large trunks - the upper (for the muscle that lifts the upper eyelid, the upper straight and upper oblique muscles) and the lower (for the rest of the oculomotor muscles). In this case, the arteries that feed the four rectus muscles of the eye, outside the tendon attachment, give branches to the sclera, called the anterior ciliary arteries (aa. ciliares anteriores), two from each muscle branch, with the exception of the external rectus muscle, which has one branch.
At a distance of 3-4 mm from the limbus, the anterior ciliary arteries begin to divide into small branches. Some of them go to the limbus of the cornea and form a two-layer marginal looped network through new branches - superficial (plexus episcleralis) and deep (plexus scleralis). Other branches of the anterior ciliary arteries perforate the wall of the eye and near the root of the iris, together with the posterior long ciliary arteries, form a large arterial circle of the iris.
The medial arteries of the eyelids (aa. palpebrales mediales) in the form of two branches (upper and lower) approach the skin of the eyelids in the region of their internal ligament. Then, lying horizontally, they widely anastomose with the lateral arteries of the eyelids (aa. palpebrales laterales), extending from the lacrimal artery (a. lacrimalis). As a result, arterial arches of the eyelids are formed - upper (arcus palpebralis superior) and lower (arcus palpebralis inferior) (Fig. 3.13). Anastomoses from a number of other arteries also participate in their formation: supraorbital (a. supraorbitalis) - branch of the eye (a. ophthalmica), infraorbital (a. infraorbitalis) - branch of the maxillary (a. maxillaris), angular (a. angularis) - branch of the facial (a. facialis), superficial temporal (a. temporalis superficialis) - a branch of the external carotid (a. carotis externa).
Both arcs are located in the muscle layer of the eyelids at a distance of 3 mm from the ciliary edge. However, the upper eyelid often has not one, but two

Rice. 3.13. Arterial blood supply to the eyelids [according to S. S. Dutton, 1994].
arterial arches. The second of them (peripheral) is located above the upper edge of the cartilage and is connected to the first by vertical anastomoses. In addition, small perforating arteries (aa. perforantes) depart from the same arcs to the posterior surface of the cartilage and conjunctiva. Together with the branches of the medial and lateral arteries of the eyelids, they form the posterior conjunctival arteries, which are involved in the blood supply to the mucous membrane of the eyelids and, in part, to the eyeball.
The supply of the conjunctiva of the eyeball is carried out by the anterior and posterior conjunctival arteries. The former depart from the anterior ciliary arteries and head towards the conjunctival fornix, while the latter, being branches of the lacrimal and supraorbital arteries, go towards them. Both of these circulatory systems are connected by many anastomoses.
The lacrimal artery (a. lacrimalis) departs from the initial part of the arc of the ophthalmic artery and is located between the external and superior rectus muscles, giving them and the lacrimal gland multiple branches. In addition, she, as indicated above, with her branches (aa. palpebrales laterales) takes part in the formation of the arterial arches of the eyelids.
The supraorbital artery (a. supraorbitalis), being a fairly large trunk of the ophthalmic artery, passes in the upper part of the orbit to the same notch in the frontal bone. Here, together with the lateral branch of the supraorbital nerve (r. lateralis n. supraorbitalis), it goes under the skin, nourishing the muscles and soft tissues of the upper eyelid.
The supratrochlear artery (a. supratrochlearis) exits the orbit near the block along with the nerve of the same name, having previously perforated the orbital septum (septum orbitale).
The ethmoid arteries (aa. ethmoidales) are also independent branches of the ophthalmic artery, but their role in the nutrition of the orbital tissues is insignificant.
From the system of the external carotid artery, some branches of the facial and maxillary arteries take part in the nutrition of the auxiliary organs of the eye.
The infraorbital artery (a. infraorbitalis), being a branch of the maxillary, enters the orbit through the inferior orbital fissure. Located subperiosteally, it passes through the canal of the same name on the lower wall of the infraorbital groove and goes to the front surface of the maxillary bone. Participates in the nutrition of the tissues of the lower eyelid. Small branches extending from the main arterial trunk are involved in the blood supply to the inferior rectus and inferior oblique muscles, the lacrimal gland and the lacrimal sac.
The facial artery (a. facialis) is a fairly large vessel located in the medial part of the entrance to the orbit. In the upper section it gives off a large branch - the angular artery (a. angularis).
3.4.2. The venous system of the organ of vision
The outflow of venous blood directly from the eyeball occurs mainly through the internal (retinal) and external (ciliary) vascular systems of the eye. The first is represented by the central retinal vein, the second - by four vorticose veins (see Fig. 3.10; 3.11).
The central retinal vein (v. centralis retinae) accompanies the corresponding artery and has the same distribution as it does. In the trunk of the optic nerve, it connects to the central artery of the network

Rice. 3.14. Deep veins of the orbit and face [according to R. Thiel, 1946].
chatki into the so-called central connecting cord through processes extending from the pia mater. It flows either directly into the cavernous sinus (sinus cavernosa), or previously into the superior ophthalmic vein (v. ophthalmica superior).
Vorticose veins (vv. vorticosae) divert blood from the choroid, ciliary processes and most of the muscles of the ciliary body, as well as the iris. They cut through the sclera in an oblique direction in each of the quadrants of the eyeball at the level of its equator. The superior pair of vorticose veins drains into the superior ophthalmic vein, the inferior pair into the inferior one.
The outflow of venous blood from the auxiliary organs of the eye and orbit occurs through the vascular system, which has a complex structure and
characterized by a number of clinically very important features (Fig. 3.14). All veins of this system are devoid of valves, as a result of which the outflow of blood through them can occur both towards the cavernous sinus, i.e., into the cranial cavity, and into the system of facial veins that are associated with the venous plexuses of the temporal region of the head, pterygoid process, and pterygopalatine fossa , condylar process of the mandible. In addition, the venous plexus of the orbit anastomoses with the veins of the ethmoid sinuses and the nasal cavity. All these features determine the possibility of a dangerous spread of purulent infection from the skin of the face (boils, abscesses, erysipelas) or from the paranasal sinuses to the cavernous sinus.
3.5. Motor
and sensory innervation
eyes and its auxiliary
bodies
Motor innervation of the human organ of vision is realized with the help of III, IV, VI and VII pairs of cranial nerves, sensitive - through the first (n. ophthalmicus) and partly second (n. maxillaris) branches of the trigeminal nerve (V pair of cranial nerves).
The oculomotor nerve (n. oculomotorius, III pair of cranial nerves) starts from the nuclei lying at the bottom of the Sylvian aqueduct at the level of the anterior tubercles of the quadrigemina. These nuclei are heterogeneous and consist of two main lateral (right and left), including five groups of large cells (nucl. oculomotorius), and additional small cells (nucl. oculomotorius accessorius) - two paired lateral (Yakubovich-Edinger-Westphal nucleus) and one unpaired (Perlia's nucleus), located between
them (Fig. 3.15). The length of the nuclei of the oculomotor nerve in the anteroposterior direction is 5-6 mm.
From the paired lateral large cell nuclei (a-d) fibers for three straight (upper, inner and lower) and lower oblique oculomotor muscles, as well as for two portions of the muscle that lifts the upper eyelid, and the fibers innervating the inner and lower straight, as well as inferior oblique muscles, immediately decussate.
The fibers extending from the paired small cell nuclei through the ciliary node innervate the muscle of the sphincter of the pupil (m. sphincter pupillae), and those extending from the unpaired nucleus - the ciliary muscle.
Through the fibers of the medial longitudinal bundle, the nuclei of the oculomotor nerve are connected with the nuclei of the trochlear and abducens nerves, the system of vestibular and auditory nuclei, the nucleus of the facial nerve and the anterior horns of the spinal cord. This ensures

Rice. 3.15. Innervation of the external and internal muscles of the eye [according to R. Bing, B. Brückner, 1959].
coordinated reflex reactions of the eyeball, head, torso to all kinds of impulses, in particular vestibular, auditory and visual.
Through the superior orbital fissure, the oculomotor nerve enters the orbit, where, within the muscular funnel, it divides into two branches - upper and lower. The upper thin branch is located between the superior rectus muscle and the muscle that lifts the upper eyelid, and innervates them. The lower, larger branch passes under the optic nerve and is divided into three branches - the outer one (the root to the ciliary node and fibers for the lower oblique muscle depart from it), the middle and the inner one (innervating the lower and inner rectus muscles, respectively). The root (radix oculomotoria) carries fibers from the accessory nuclei of the oculomotor nerve. They innervate the ciliary muscle and the sphincter of the pupil.
Block nerve (n. trochlearis, IV pair of cranial nerves) starts from the motor nucleus (length 1.5-2 mm), located at the bottom of the Sylvian aqueduct immediately behind the nucleus of the oculomotor nerve. Penetrates into the orbit through the superior orbital fissure lateral to the muscular infundibulum. Innervates the superior oblique muscle.
Abducens nerve (n. abducens, VI pair of cranial nerves) starts from the nucleus located in the pons at the bottom of the rhomboid fossa. It leaves the cranial cavity through the superior orbital fissure, located inside the muscular funnel between the two branches of the oculomotor nerve. Innervates the external rectus muscle of the eye.
The facial nerve (n. facialis, n. intermediofacialis, VII pair of cranial nerves) has a mixed composition, that is, it includes not only motor, but also sensory, gustatory and secretory fibers that belong to the intermediate
nerve (n. intermedius Wrisbergi). The latter is closely adjacent to the facial nerve at the base of the brain from the outside and is its posterior root.
The motor nucleus of the nerve (length 2-6 mm) is located in the lower part of the pons varolii at the bottom of the IV ventricle. The fibers departing from it exit in the form of a root to the base of the brain in the cerebellopontine angle. Then the facial nerve, together with the intermediate one, enters the facial canal of the temporal bone. Here they merge into a common trunk, which further penetrates the parotid salivary gland and divides into two branches, forming the parotid plexus - plexus parotideus. Nerve trunks depart from it to the facial muscles, including the circular muscle of the eye.
The intermediate nerve contains secretory fibers for the lacrimal gland. They depart from the lacrimal nucleus located in the brain stem and through the knee node (gangl. geniculi) enter the large stony nerve (n. petrosus major).
The afferent pathway for the main and accessory lacrimal glands begins with the conjunctival and nasal branches of the trigeminal nerve. There are other zones of reflex stimulation of tear production - the retina, the anterior frontal lobe of the brain, the basal ganglion, the thalamus, the hypothalamus and the cervical sympathetic ganglion.
The level of damage to the facial nerve can be determined by the state of secretion of the lacrimal fluid. When it is not broken, the center is below gangl. geniculi and vice versa.
The trigeminal nerve (n. trigeminus, V pair of cranial nerves) is mixed, that is, it contains sensory, motor, parasympathetic and sympathetic fibers. It distinguishes nuclei (three sensitive - spinal, bridge, midbrain - and one motor), sensitive and motor-
telny roots, as well as the trigeminal node (on the sensitive root).
Sensitive nerve fibers start from bipolar cells of a powerful trigeminal ganglion (gangl. trigeminale) 14-29 mm wide and 5-10 mm long.
The axons of the trigeminal ganglion form the three main branches of the trigeminal nerve. Each of them is associated with certain nerve nodes: the ophthalmic nerve (n. ophthalmicus) - with the ciliary (gangl. ciliare), the maxillary (n. maxillaris) - with the pterygopalatine (gangl. pterygopalatinum) and the mandibular (n. mandibularis) - with the ear ( gangl. oticum), submandibular (gangl. submandibulare) and sublingual (gangl. sublihguale).
The first branch of the trigeminal nerve (n. ophthalmicus), being the thinnest (2-3 mm), exits the cranial cavity through the fissura orbitalis superior. When approaching it, the nerve is divided into three main branches: n. nasociliaris, n. frontalis and n. lacrimalis.
N. nasociliaris, located within the muscular funnel of the orbit, in turn is divided into long ciliary, ethmoid and nasal branches and gives, in addition, the root (radix nasociliaris) to the ciliary node (gangl. ciliare).
Long ciliary nerves in the form of 3-4 thin trunks are sent to the posterior pole of the eye, perforate
sclera in the circumference of the optic nerve and along the suprachoroidal space are directed anteriorly. Together with short ciliary nerves extending from the ciliary ganglion, they form a dense nerve plexus in the region of the ciliary body (plexus ciliaris) and around the circumference of the cornea. The branches of these plexuses provide sensitive and trophic innervation of the corresponding structures of the eye and the perilimbal conjunctiva. The rest of it receives sensitive innervation from the palpebral branches of the trigeminal nerve, which should be borne in mind when planning anesthesia of the eyeball.
On the way to the eye, sympathetic nerve fibers from the plexus of the internal carotid artery join the long ciliary nerves, which innervate the pupil dilator.
Short ciliary nerves (4-6) depart from the ciliary node, the cells of which are connected with the fibers of the corresponding nerves through sensory, motor and sympathetic roots. It is located at a distance of 18-20 mm behind the posterior pole of the eye under the external rectus muscle, adjacent in this zone to the surface of the optic nerve (Fig. 3.16).
Like the long ciliary nerves, the short ones also approach the posterior

Rice. 3.16. The ciliary ganglion and its innervation connections (scheme).
pole of the eye, perforate the sclera along the circumference of the optic nerve and, increasing in number (up to 20-30), participate in the innervation of the tissues of the eye, primarily its choroid.
Long and short ciliary nerves are a source of sensory (cornea, iris, ciliary body), vasomotor and trophic innervation.
Terminal branch n. nasociliaris is the subtrochlear nerve (n. infratrochlearis), which innervates the skin in the root of the nose, the inner corner of the eyelids and the corresponding parts of the conjunctiva.
The frontal nerve (n. frontalis), being the largest branch of the optic nerve, after entering the orbit, gives off two large branches - the supraorbital nerve (n. supraorbitalis) with the medial and lateral branches (r. medialis et lateralis) and the supratrochlear nerve. The first of them, having perforated the tarsoorbital fascia, passes through the nasopharyngeal foramen (incisura supraorbital) of the frontal bone to the skin of the forehead, and the second leaves the orbit at its inner wall and innervates a small area of the skin of the eyelid above its internal ligament. In general, the frontal nerve provides sensory innervation to the middle part of the upper eyelid, including the conjunctiva, and the skin of the forehead.
The lacrimal nerve (n. lacrimalis), entering the orbit, goes anteriorly over the external rectus muscle of the eye and is divided into two branches - the upper (larger) and lower. The upper branch, being a continuation of the main nerve, gives branches to
lacrimal gland and conjunctiva. Some of them, after passing through the gland, perforate the tarsoorbital fascia and innervate the skin in the region of the outer corner of the eye, including the area of the upper eyelid. A small lower branch of the lacrimal nerve anastomoses with the zygomatic-temporal branch (r. zygomaticotemporalis) of the zygomatic nerve, which carries secretory fibers for the lacrimal gland.
The second branch of the trigeminal nerve (n. maxillaris) takes part in the sensitive innervation of only the auxiliary organs of the eye through its two branches - n. infraorbitalis and n. zygomaticus. Both of these nerves separate from the main trunk in the pterygopalatine fossa and enter the orbital cavity through the inferior orbital fissure.
The infraorbital nerve (n. infraorbitalis), entering the orbit, passes along the groove of its lower wall and exits through the infraorbital canal to the front surface. Innervates the central part of the lower eyelid (rr. palpebrales inferiores), the skin of the wings of the nose and the mucous membrane of its vestibule (rr. nasales interni et externi), as well as the mucous membrane of the upper lip (rr. labiales superiores), upper gum, alveolar depressions and, in addition in addition, the upper dentition.
The zygomatic nerve (n. zygomaticus) in the cavity of the orbit is divided into two branches - n. zygomaticotemporalis and n. zygomaticofacialis. Having passed through the corresponding channels in the zygomatic bone, they innervate the skin of the lateral part of the forehead and a small area of the zygomatic region.
The organ of vision is one of the main sense organs, it plays a significant role in the process of perceiving the environment. In the diverse activities of man, in the performance of many of the most delicate works, the organ of vision is of paramount importance. Having reached perfection in a person, the organ of vision captures the light flux, directs it to special light-sensitive cells, perceives black and white and color image sees an object in volume and at different distances.
The organ of vision is located in the orbit and consists of an eye and an auxiliary apparatus (Fig. 144).
Rice. 144. The structure of the eye (diagram):
1 - sclera; 2 - choroid; 3 - retina; 4 - central fossa; 5 - blind spot; 6 - optic nerve; 7 - conjunctiva; 8 - ciliary ligament; 9—cornea; 10—pupil; 11, 18 - optical axis; 12 - anterior chamber; 13 - lens; 14 - iris; 15 - rear camera; 16 - ciliary muscle; 17 - vitreous body
The eye (oculus) consists of the eyeball and the optic nerve with its membranes. The eyeball has a rounded shape, anterior and posterior poles. The first corresponds to the most protruding part of the outer fibrous membrane (cornea), and the second corresponds to the most protruding part, which is the lateral exit of the optic nerve from the eyeball. The line connecting these points is called the outer axis of the eyeball, and the line connecting the point on the inner surface of the cornea with the point on the retina is called the inner axis of the eyeball. Changes in the ratio of these lines cause disturbances in the focus of the image of objects on the retina, the appearance of myopia (myopia) or farsightedness (hypermetropia).
The eyeball consists of the fibrous and choroid membranes, the retina and the nucleus of the eye (the aqueous humor of the anterior and posterior chambers, the lens, the vitreous body).
The fibrous sheath is an outer dense sheath that performs protective and light-transmitting functions. The anterior part is called the cornea, the posterior part is called the sclera. The cornea is the transparent part of the shell, which has no blood vessels, and is shaped like a watch glass. The corneal diameter is 12 mm, thickness is about 1 mm.
The sclera consists of dense fibrous connective tissue, about 1 mm thick. On the border with the cornea in the thickness of the sclera there is a narrow channel - the venous sinus of the sclera. The oculomotor muscles are attached to the sclera.
The choroid contains a large number of blood vessels and pigment. It consists of three parts: own choroid, ciliary body and iris. The choroid proper forms most of the choroid and lines the back of the sclera, fuses loosely with the outer shell; between them is the perivascular space in the form of a narrow gap.
The ciliary body resembles a moderately thickened section of the choroid, which lies between its own choroid and the iris. The basis of the ciliary body is loose connective tissue, rich in blood vessels and smooth muscle cells. The anterior section has about 70 radially arranged ciliary processes that make up the ciliary crown. Radially located fibers of the ciliary belt are attached to the latter, which then go to the anterior and posterior surfaces of the lens capsule. The posterior part of the ciliary body - the ciliary circle - resembles thickened circular stripes that pass into the choroid. The ciliary muscle consists of intricately intertwined bundles of smooth muscle cells. With their contraction, a change in the curvature of the lens and adaptation to a clear vision of the object (accommodation) occur.
The iris is the most anterior part of the choroid, has the shape of a disk with a hole (pupil) in the center. It consists of connective tissue with vessels, pigment cells that determine the color of the eyes, and muscle fibers arranged radially and circularly.
In the iris, the anterior surface, which forms the posterior wall of the anterior chamber of the eye, and the pupillary margin, which encloses the pupillary opening, are distinguished. The posterior surface of the iris constitutes the anterior surface of the posterior chamber of the eye; the ciliary margin is connected to the ciliary body and sclera by the pectinate ligament. Muscle fibers of the iris, contracting or relaxing, reduce or increase the diameter of the pupils.
The inner (sensitive) shell of the eyeball - the retina - fits snugly against the vascular. The retina has a large posterior visual part and a smaller anterior "blind" part, which combines the ciliary and iris parts of the retina. The visual part consists of the internal pigment and internal nervous parts. The latter has up to 10 layers of nerve cells. In inner part The retina includes cells with processes in the form of cones and rods, which are the light-sensitive elements of the eyeball. Cones perceive light rays in bright (daylight) light and are simultaneously color receptors, while rods function in twilight lighting and play the role of twilight light receptors. The remaining nerve cells perform a connecting role; the axons of these cells, united in a bundle, form a nerve that exits the retina.
In the posterior part of the retina there is a kind of exit of the optic nerve - the optic disc, and the yellowish spot is located lateral to it. Here is the largest number of cones; this something is the epitome of the greatest vision.
The nucleus of the eye includes the anterior and posterior chambers filled with aqueous humor, the lens and the vitreous body. The anterior chamber of the eye is the space between the cornea at the front and the anterior surface of the iris at the back. Something along the circumference, where the edge of the cornea and iris is located, is limited by the pectinate ligament. Between the bundles of this ligament is the space of the iris-corneal node (fountain spaces). Through these spaces, aqueous humor from the anterior chamber flows into the venous sinus of the sclera (Schlemm's canal), and then enters the anterior ciliary veins. Through the opening of the pupil, the anterior chamber is connected to the posterior chamber of the eyeball. The posterior chamber, in turn, is connected to the spaces between the fibers of the lens and the ciliary body. Along the periphery of the lens lies a space in the form of a girdle (petite canal) filled with aqueous humor.
The lens is a biconvex lens that is located behind the chambers of the eye and has a light refractive ability. It distinguishes between the anterior and posterior surfaces and the equator. The substance of the lens is colorless, transparent, dense, has no vessels and nerves. Its inner part - the core - is much denser than the peripheral part. Outside, the lens is covered with a thin transparent elastic capsule, to which the ciliary girdle (zinn ligament) is attached. When the ciliary muscle contracts, the size of the lens and its refractive power change.
The vitreous body is a jelly-like transparent mass that has no vessels and nerves and is covered with a membrane. It is located in the vitreous chamber of the eyeball, behind the lens and fits snugly against the retina. On the side of the lens in the vitreous body is a depression called the vitreous fossa. The refractive power of the vitreous body is close to that of the aqueous humor that fills the chambers of the eye. In addition, the vitreous body performs supporting and protective functions.
Accessory organs of the eye. The auxiliary organs of the eye include the muscles of the eyeball (Fig. 145), the fascia of the orbit, the eyelids, the eyebrows, the lacrimal apparatus, the fatty body, the conjunctiva, the vagina of the eyeball. 

Rice. 145. Muscles of the eyeball:
A - view from the lateral side: 1 - superior rectus muscle; 2 - the muscle that lifts the upper eyelid; 3 - lower oblique muscle; 4 - lower straight muscle; 5 - lateral rectus muscle; B - top view: 1 - block; 2 - sheath of the tendon of the superior oblique muscle; 3 - superior oblique muscle; 4 - medial rectus muscle; 5 - lower straight muscle; 6 - upper straight muscle; 7 - lateral rectus muscle; 8 - muscle that lifts the upper eyelid
The motor apparatus of the eye is represented by six muscles. Muscles originate from the tendon ring around the optic nerve at the back of the eye socket and attach to the eyeball. There are four rectus muscles of the eyeball (upper, lower, lateral and medial) and two oblique (upper and lower). The muscles act in such a way that both eyes turn in concert and are directed to the same point. From the tendon ring also begins the muscle that lifts the upper eyelid. The muscles of the eye are striated muscles and contract voluntarily.
The orbit, in which the eyeball is located, consists of the periosteum of the orbit, which fuses with the hard shell of the brain in the region of the optic canal and the superior orbital fissure. The eyeball is covered with a shell (or Tenon's capsule), which is loosely connected to the sclera and forms the episcleral space. Between the vagina and the periosteum of the orbit is the fatty body of the orbit, which acts as an elastic cushion for the eyeball.
The eyelids (upper and lower) are formations that lie in front of the eyeball and cover it from above and below, and when closed, they completely close it. The eyelids have an anterior and posterior surface and free edges. The latter, connected by spikes, form the medial and lateral corners of the eye. In the medial corner are the lacrimal lake and the lacrimal meat. On the free edge of the upper and lower eyelids near the medial angle, a slight elevation is visible - the lacrimal papilla with a hole at the top, which is the beginning of the lacrimal canaliculus.
The space between the edges of the eyelids is called the palpebral fissure. Eyelashes are located along the front edge of the eyelids. The basis of the eyelid is cartilage, which is covered with skin on top, and with inside- the conjunctiva of the eyelid, which then passes into the conjunctiva of the eyeball. The recess that forms when the conjunctiva of the eyelids passes to the eyeball is called the conjunctival sac. The eyelids, in addition to the protective function, reduce or block the access of the light flux.
On the border of the forehead and upper eyelid there is an eyebrow, which is a roller covered with hair and performing a protective function.
The lacrimal apparatus consists of the lacrimal gland with excretory ducts and lacrimal ducts. The lacrimal gland is located in the fossa of the same name in the lateral angle, near the upper wall of the orbit and is covered with a thin connective tissue capsule. The excretory ducts (there are about 15 of them) of the lacrimal gland open into the conjunctival sac. A tear washes the eyeball and constantly moisturizes the cornea. The movement of tears is facilitated by the blinking movements of the eyelids. Then the tear flows through the capillary gap near the edge of the eyelids into the lacrimal lake. In this process, the lacrimal ducts originate, which open into the lacrimal sac. The latter is located in the fossa of the same name in the lower medial corner of the orbit. From top to bottom, it passes into a rather wide nasolacrimal canal, through which the lacrimal fluid enters the nasal cavity.
Conducting paths of the visual analyzer (Fig. 146). The light that enters the retina first passes through the transparent light-refracting apparatus of the eye: the cornea, the aqueous humor of the anterior and posterior chambers, the lens and the vitreous body. The beam of light on its way is regulated by the pupil. The refractive apparatus directs a beam of light to a more sensitive part of the retina - something of the best vision - a spot with its central fovea. Passing through all the layers of the retina, light causes complex photochemical transformations of visual pigments there. As a result, a nerve impulse arises in light-sensitive cells (rods and cones), which is then transmitted to the next retinal neurons - bipolar cells (neurocytes), and after them - neurocytes of the ganglionic layer, ganglionic neurocytes. The processes of the latter go towards the disc and form the optic nerve. Having passed into the skull through the optic nerve canal along the lower surface of the brain, the optic nerve forms an incomplete optic chiasm. From the optic chiasm begins the optic tract, which consists of the nerve fibers of the ganglion cells of the retina of the eyeball. Then the fibers along the optic tract go to the subcortical visual centers: the lateral geniculate body and the superior mounds of the roof of the midbrain. In the lateral geniculate body, the fibers of the third neuron (ganglion neurocytes) of the visual pathway end and come into contact with the cells of the next neuron. The axons of these neurocytes pass through the internal capsule and reach the cells of the occipital lobe near the spur groove, where they end (the cortical end of the visual analyzer). Part of the axons of ganglion cells pass through the geniculate body and, as part of the handle, enters the superior colliculus. Further, from the gray layer of the upper colliculus, impulses go to the nucleus of the oculomotor nerve and to the additional nucleus, from where the innervation of the oculomotor muscles, the muscles that constrict the pupils, and the ciliary muscle occurs. These fibers carry an impulse in response to light stimulation and the pupils constrict (pupillary reflex), and a turn in the necessary direction of the eyeballs also occurs.

Rice. 146. Scheme of the structure of the visual analyzer:
1 - retina; 2 - uncrossed fibers of the optic nerve; 3 - crossed fibers of the optic nerve; 4 - visual tract; 5 - cortical analyzer
The mechanism of photoreception is based on the gradual transformation of the visual pigment rhodopsin under the action of light quanta. The latter are absorbed by a group of atoms (chromophores) of specialized molecules - chromolipoproteins. As a chromophore, which determines the degree of light absorption in visual pigments, aldehydes of vitamin A alcohols, or retinal, act. The latter are always in the form of 11-cisretinal and normally bind to the colorless protein opsin, thus forming the visual pigment rhodopsin, which, through a series of intermediate stages, is again cleaved into retinal and opsin. In this case, the molecule loses color and this process is called fading. The scheme of transformation of the rhodopsin molecule is presented as follows.

The process of visual excitation occurs in the period between the formation of lumi- and metarhodopsin II. After the cessation of exposure to light, rhodopsin is immediately resynthesized. At first, completely with the participation of the enzyme retinal isomerase, trans-retinal is converted into 11-cisretinal, and then the latter combines with opsin, again forming rhodopsin. This process is continuous and underlies dark adaptation. In complete darkness, it takes about 30 minutes for all the rods to adapt and the eyes to acquire maximum sensitivity. Image formation in the eye occurs with the participation of optical systems (cornea and lens), which give an inverted and reduced image of an object on the surface of the retina. The adaptation of the eye to see clearly at a distance of distant objects is called accommodation. The mechanism of accommodation of the eye is associated with the contraction of the ciliary muscles, which change the curvature of the lens.
When considering objects at a close distance, convergence also acts simultaneously with accommodation, i.e., the axes of both eyes converge. The visual lines converge the more, the closer the object under consideration is.
The refractive power of the optical system of the eye is expressed in diopters ("D" - diopter). For 1 D, the power of a lens is taken, the focal length of which is 1 m. The refractive power of the human eye is 59 diopters when considering distant objects and 70.5 diopters when considering close ones.
There are three main anomalies in the refraction of rays in the eye (refraction): myopia, or myopia; farsightedness, or hypermetropia; senile farsightedness, or presbyopia (Fig. 147). The main cause of all eye defects is that the refractive power and the length of the eyeball do not agree with each other, as in a normal eye. With myopia (myopia), the rays converge in front of the retina in the vitreous body, and on the retina at some point a circle of light scattering appears, while the eyeball is longer than normal. Concave lenses with negative diopters are used to correct vision.


Rice. 147. The course of light rays in a normal eye (A), with myopia
(B1 and B2), with farsightedness (B1 and C2) and with astigmatism (G1 and G2):
B2, B2 - biconcave and biconvex lenses for correcting defects of myopia and hyperopia; G2 - cylindrical lens for the correction of astigmatism; 1 - zone of clear vision; 2 - blurred image area; 3 - corrective lenses
With farsightedness (hypermetropia), the eyeball is short, and therefore parallel rays coming from distant objects are collected behind the retina, and an obscure, blurry image of the object is obtained on it. This disadvantage can be compensated by using the refractive power of convex lenses with positive diopters.
Senile farsightedness (presbyopia) is associated with a weak elasticity of the lens and a weakening of the tension of the zonn ligaments with a normal length of the eyeball.
This refractive error can be corrected with biconvex lenses. Vision with one eye gives us an idea of the object in only one plane. Only when seeing simultaneously with two eyes is it possible to perceive depth and correctly understand the relative position of objects. The ability to merge individual images received by each eye into a single whole provides binocular vision.
Visual acuity characterizes the spatial resolution of the eye and is determined by the smallest angle at which a person is able to distinguish two points separately. The smaller the angle, the better the vision. Normally, this angle is 1 min, or 1 unit.
To determine visual acuity, special tables are used, which show letters or figures of various sizes.
The field of view is the space that is perceived by one eye when it is stationary. A change in visual field can be an early sign of some eye and brain disorders.
Color perception is the ability of the eye to distinguish colors. Thanks to this visual function, a person is able to perceive about 180 color shades. Color vision is of great practical importance in a number of professions, especially in the arts. Like visual acuity, color perception is a function of the cone apparatus of the retina. Color vision disorders can be congenital and inherited and acquired.
Violation of color perception is called color blindness and is determined using pseudo-isochromatic tables, which represent a set of colored dots that form a sign. A person with normal vision easily distinguishes the contours of the sign, but a color-blind person does not.
The human body is a complex system in which all elements are closely interconnected and the work of some organs is simply impossible without the functioning of others. For example, sense organs or analyzers allow not only to explore and perceive the surrounding world, but are also the primary link in self-consciousness, creativity and other complex mental processes. The eyes are the most significant sensory organ, since we receive more than 90% of information through vision. They have a complex anatomy and are a natural optical system that can adapt to any external conditions.
The eye as an organ
Like any analyzer, the eye includes three main elements:
- The peripheral part, whose task is to read visual stimuli and recognize them;
- Nervous pathways through which information enters the central nervous system;
- The part of the brain where the analysis and interpretation of all the information received is carried out. Processing of visual stimuli occurs in the occipital region of each hemisphere.
Despite the development of modern medicine, analyzers have not yet been fully explored. This is largely due to their complex structure and direct connection with the brain - the most unexplored organ of the human body.
The peripheral part of the human visual analyzer is the eyeball located in the orbit or eye socket, which protects it from damage and injury. Its full-fledged work is provided by the optic nerve, 6 muscles of various purposes, the protective system (eyelids, eyelashes, glands), as well as the system of blood vessels. The eyeball itself has a spherical shape with a volume of up to 7 cm 3 and a mass of up to 78 grams. From an anatomical point of view, the eye includes 3 shells - fibrous, vascular and retina.

The structure of the eye
Basic structures
The fibrous membrane is represented by the sclera, cornea and limbus - the place where one part passes into another
Sclera
The most voluminous element of the fibrous membrane (80% of the total volume). It consists of dense connective tissue, necessary for fixing the eye muscles. It is the sclera that allows you to maintain the tone and shape of the eyeball. In the posterior pole there is a kind of lattice surface necessary for innervation. In fact, the sclera is a framework for all other elements of the eyeball. 

Cornea
This colorless element of the fibrous membrane is much smaller than other structures in size. A healthy cornea is a transparent spherical element, up to 0.4 mm thick, with a pronounced luster and high photosensitivity. Its main task is to refract and conduct beams of light.. The refractive power of this structure in a healthy person is 40 diopters. 
Nutrition and cellular metabolism in the eyeball is supported by the middle or choroid. It is represented by the iris, the ciliary body, and the system of blood vessels (choroid).
iris
It is located directly behind the cornea of the eyeball and has a pupil in the very center - a self-regulating hole, 2-8 mm in diameter, which acts as a diaphragm. Melanin is responsible for the color of the iris. Its task is to protect the eye from excess sunlight. 
Ciliary (ciliary) body
This is a small area located at the base of the iris. In its thickness is a muscle that provides curvature and focusing of the lens. It is the ciliary muscle that is the key in the process of accommodation of the eye. 
choroid
This is the choroid of the eye, the task of which is to provide nutrition to all structural elements. In addition, she takes an active part in the regeneration of visual substances decaying over time. 
lens
This element is located immediately behind the pupil. In fact, it is a natural lens, which, due to the ciliary body, can change its curvature and take part in focusing on objects of different distances. Its refractive power is from 20 to 30 diopters, depending on muscle tone. 
Retina
This is the light-sensitive shell of the eye, with a thickness of 0.07 to 0.5 mm, which are represented by 10 different layers of cells. Some anatomists compare the retina to the film of a camera, because its main task is to form an image using cones and rods (specialized light-sensitive cells). The rods are located on the peripheral part of the retina and are responsible for twilight and black-and-white vision, and the cones located in the central zone are the macula (yellow spot). 
Auxiliary elements
Many researchers combine additional auxiliary elements of the eye into one group. As a rule, this includes eyelashes, eyelids with a thin mucous membrane (conjunctiva) lining it from the inside, in the thickness of which the lacrimal glands are located. Their main task is to protect the eyeball from mechanical stress, dust and dirt. 
The eye is a complex mechanism in which all parts work synchronously and cannot do without each other. That is why ophthalmic diseases are so often accompanied by complications, because if the functioning of one element is disrupted, others experience difficulties.
Optical system
The main task of the visual analyzer is to obtain a clear and crisp image, which is then sent through the nerve fibers to the brain, where the information is analyzed. Contrary to popular belief, we do not see the object itself, but only the rays reflected from it, which are subsequently focused on the surface of the retina. Before hitting the retina, light rays travel a complex and long path that lies through 3 refractive surfaces - the cornea, lens and vitreous body. 
The process of refraction of light rays in the human eye system is called refraction, and the mechanism itself is described in detail in optics.
Refraction in the eyeball occurs exactly 4 times. First, a beam of light is refracted in the anterior and posterior sections of the cornea, then into the lens and is slightly refracted by liquid internal media. Visual acuity directly depends on the refractive power of these elements. The average refractive power of the human eye is 60 diopters (59 D when distinguishing distant objects and 70.5 D nearby).
On the retina, the image appears greatly reduced, turned upside down and projected from right to left. Subsequent object recognition already occurs in the occipital region of the brain.
There are 3 main characteristics of the human optical system:
- binocular vision. Perception of the image of objects simultaneously with two eyes, while normally not feeling duality. It is believed that always one eye is the leader, and the second is the slave;
- stereoscopic. The ability to see not flat, but three-dimensional images, in other words, the human eye can estimate the distance to the object, its true shape, as well as its real size;
- Visual acuity. Thanks to it, it is possible to recognize two points that are equidistant from each other.
Due to the presence of light-sensitive cells - cones, the visual analyzer is able to distinguish the colors of objects. This possibility is not present in all species of mammals.
Age development of the visual analyzer and its optical power
The rudiments of the visual system appear at the 3rd week of embryonic development, and the formation of vision is completed only at 12-14 years. In newborns, you may notice excessive bulging of the eyeballs due to the unformed size of the orbit. Up to 2 years, the eye increases in size by 40%, and by 5 years by 70% of its original volume. In addition, in the first years of life, the cornea is much thicker, and the lens has greater elasticity, but this disappears as the nucleus develops. With pathologies, ophthalmic disorders occur in the form.
After 14 years, eye structures practically do not change, the depletion of structural elements begins after 45-50 years, depending on individual characteristics. With age, the refraction of the lens changes, which leads to the development of or.
Central vision occurs only at 2-3 months of a person's life and in the future it is constantly being improved. First, the ability to distinguish objects arises, and with the development of the intellect, the ability to recognize them also appears. By 6 months, the newborn can respond to the appearance of familiar faces, by the end of the first year, the ability to recognize simple geometric shapes appears. Only by the age of 2-3 years does the ability to recognize painted images of objects develop. Full perception of shapes and sizes, as well as normal visual acuity, are observed only by 6-7 years. Including, therefore, it is inappropriate to send the child to study earlier than this period. 
The visual acuity of the baby is very small and is 0.002-0.03. By the age of 2, it rises to 0.4-0.7, and by the age of 5-7 it returns to normal (0.8-1.0). Newborn children see objects upside down for a long time until the visual cortex of the cerebral hemispheres develops sufficiently.
At birth, the child has no conscious vision at all. His eyes are only able to react to bright light by constricting the pupils, and the eyeballs themselves move asynchronously independently of each other. That is why binocular vision develops much later than other visual functions.
Adaptation
The human eye is able to adapt to lighting conditions, thanks to which we can distinguish objects under different light sources. This visual function is called adaptation. It is possible due to a change in the size of the pupil, due to which the ability to transmit light changes, as well as a different photochemical reaction of rods and cones. Full contraction of the pupil occurs within 5 seconds, and the maximum expansion lasts up to 5 minutes. There are three types of adaptation:
- color. Provides correct perception of color depending on external conditions;
- Dark. Occurs when moving from the highest brightness to the lowest. Full sensitivity of the eye to darkness is observed after 1 hour of exposure to poor lighting conditions. The ability to distinguish and see objects in the dark is provided by the expansion of the pupil and the functioning of the rods;
- Luminous. Occurs when moving from low to high brightness. During this process, the rapid decomposition of rhodopsin in the rods occurs, and the cones, on the contrary, actively gain the enzyme. Thus, blinding is a photochemical reaction. Light adaptation normally lasts no more than 10 minutes.

Different people have different rates of the mechanism of production and decomposition of rhodopsin in rods and cones. That is why some see well in the dark.
Accommodation
It is understood as the ability of a person to see objects equally well near and at a long distance, as well as quick focusing of vision when looking from one object to another. The process is automatic and uncontrollable. The signal for the start of accommodation is a fuzzy image of an object on the retina, after which the ciliary muscles and zinn ligaments, under the influence of a signal from the brain, begin to contract or relax, activating the lens. In old age, the ability to accommodate weakens due to a decrease in the elasticity of the lens and compaction of the muscle accommodation fibers. 
During focusing on nearby objects, the muscles tense up, and on distant objects, they relax. That is why it is so important from time to time to look from one object to another during work that requires long-term concentration of vision. This simple exercise allows you to change the load on the visual muscles.
Visual acuity
This is one of the main characteristics of the visual system, which is provided by many structural elements of the eye. It consists in the ability of the eyes to perceive points equidistant from each other. Its value is inversely proportional to the angle of central vision, the smaller it is, the more accurately we see objects. Normally, the eye should separately perceive objects that are 1 minute of arc away (0.016 degrees). To diagnose this parameter, use Simultaneous check according to the table of Sivtsev and Golovin
During life, visual functions deteriorate greatly due to the anatomical features of this organ. Therefore, you need to monitor eye health from a young age in order to protect yourself from the development of serious diseases. There are a number of ways to maintain eye health and visual acuity for a long time.
Hygiene
These are the factors that you should pay attention to in order to protect your eyes from, reduce the risk of vision loss. 
- It is necessary to read and work in proper lighting in order to create comfortable conditions for the eyes. It should not be too bright, but not dim;
- While reading, it is desirable to place the light behind, as if from behind the shoulder. It is recommended to keep the document at a distance of 30-35 cm from the eyes, while working at the monitor for a long time - 50-60 cm;
- It is necessary to constantly monitor the hydration of the mucous membrane. This provides maximum protection against the ingress of dust and dirt, and also reduces the likelihood of injury to the conjunctiva. Moisturizing drops can be used to avoid excessive dryness;
- Eyes get tired after about 45-50 minutes of intensive work. To reduce muscle tension, you need to take breaks and visual gymnastics;
- Do not touch your eyes with unwashed hands. During this, pathogens can be introduced, which will lead to infection. Plus, it is recommended to wash your eyes twice a day;
- In summer, sunglasses should be worn to avoid the harmful effects of ultraviolet radiation;
- If any signs of the disease appear, you do not need to delay visiting an ophthalmologist. Treatment is much more effective in the early stages.
Exercises
Competent rest of the eyes is an important condition for maintaining visual acuity and this can provide. If it is not possible to take a break during work, you can perform simple exercises that can reduce the tension of the visual apparatus. 
- Blink at high speed for 2 minutes. The rhythm can be changed, makes different pauses between blinking;
- Move your gaze to the furthest object in your field of vision. Stare at it for 30 seconds, then switch to another object. Repeat the action several times;
- Close your eyes tightly for 5-7 seconds, and then open them as wide as possible. Do 10 reps;
- Using three fingers of each hand, pinch the upper eyelids. Hold them in sufficient tension for about 2-4 seconds, and then relax. Repeat the exercise 3 times.
During the morning and evening washing, it is useful to do hydromassage of the eyes with a gentle jet of water.
Video
The organ of vision is the most important of the sense organs. It provides a person with up to 90% of information. The organ of vision is closely connected with the brain. The light-sensitive membrane of the organ of vision develops from the brain tissue.
The organ of vision, which is the peripheral part of the visual analyzer, consists of the eyeball (eye) and auxiliary organs of the eye, which are located in the orbit.
Rice. 93. Scheme of the structure of the eyeball: 1 - fibrous membrane (sclera), 2 - choroid itself, 3 - retina, 4 - iris, 5 - pupil, 6 - cornea, 7 - lens, 8 - anterior chamber of the eyeball, 9 - posterior chamber of the eyeball, 10 - ciliary girdle, 11 - ciliary body, 12 - vitreous body, 13 - spot (yellow), 14 - optic disc, 15 - optic nerve. The solid line is the outer axis of the eye, the dotted line is the visual axis of the eye
Eyeball has a spherical shape. It consists of three shells and a nucleus (Fig. 93). The outer shell is fibrous, the middle one is vascular, the inner one is photosensitive, reticulate (retina). The nucleus of the eyeball includes the lens, the vitreous body and a liquid medium - aqueous humor.
Fibrous membrane - thick, dense, represented by two sections: anterior and posterior. The anterior section occupies the surface of the eyeball; it is formed by a transparent, convex anteriorly cornea. The cornea is devoid of blood vessels and has high light refractive properties. Posterior fibrous membrane albuginea resembles the color of boiled protein chicken egg. The albuginea is formed by dense fibrous connective tissue.
choroid located under the protein and consists of three parts that are different in structure and function: the choroid itself, the ciliary body and the iris.
The choroid itself occupies most of the back of the eye. It is thin, rich in blood vessels, contains pigment cells that give it a dark brown color.
ciliary body is anterior to the choroid proper and looks like a roller. Outgrowths extend from the anterior edge of the ciliary body to the lens - ciliary processes and thin fibers (ciliary girdle) attached to the lens capsule along its equator. Most of the ciliary body consists of ciliary muscle. With its contraction, this muscle changes the tension of the fibers of the ciliary girdle and thereby regulates the curvature of the lens, changing its refractive power.
Iris, or iris, located between the cornea in front and the lens behind. It looks like a frontally located disk with a hole (pupil) in the middle. With its outer edge, the iris passes into the ciliary body, and with its inner, free edge, it limits the opening of the pupil. The connective tissue base of the iris contains blood vessels, smooth muscle and pigment cells. The color of the eyes depends on the amount and depth of the pigment - brown, black (if there is a large amount of pigment), blue, greenish (if there is little pigment). The bundles of smooth muscle cells have a double direction and form muscle that dilates the pupil And muscle that constricts the pupil. These muscles regulate the amount of light entering the eye.
Retina, or retina, adjoins from within to a choroid. The retina is divided into two parts: the posterior visual and front eyelash and iris. In the back of the visual part are laid light-sensitive cells - photoreceptors. Anterior part of the retina (blind) adjacent to the ciliary body and the iris. It does not contain photosensitive cells.
visual part of the retina has a complex structure. It consists of two sheets: inner - photosensitive and outer - pigment. The cells of the pigment layer are involved in the absorption of light that enters the eye and passes through the photosensitive layer of the retina. The inner layer of the retina consists of nerve cells located in three layers: the outer one, adjacent to the pigment layer, is photoreceptor, the middle one is associative, and the inner one is ganglionic.
photoreceptor layer of the retina comprises neurosensory rod-shaped And cone cells, whose outer segments (dendrites) are shaped sticks or cones. The disk-like structures of rod-shaped and cone-shaped neurocytes (rods and cones) contain molecules photopigments: in rods - sensitive to light (black and white), in cones - sensitive to red, green and blue light. The number of cones in the human retina reaches 6-7 million, and the number of rods is 20 times more. Rods perceive information about the shape and illumination of objects, and cones perceive colors.
The central processes (axons) of neurosensory cells (rods and cones) transmit visual impulses biopolar, cells, the second cellular layer of the retina, which are in contact with the ganglionic neurocytes of the third (ganglionic) layer of the retina.
Ganglion layer consists of large neurocytes, the axons of which form optic nerve.
In the back of the retina, two areas stand out - blind and yellow spots. blind spot is the exit point of the optic nerve from the eyeball. Here the retina does not contain photosensitive elements. Yellow spot located in the region of the posterior pole of the eye. This is the most light-sensitive part of the retina. Its middle is deepened and received the name central fossa. The line connecting the middle of the anterior pole of the eye with the fovea is called optical axis of the eye. For better vision, the eye is set so that the object under consideration and the central fossa are on the same axis.
As already noted, the nucleus of the eyeball includes the lens, vitreous body and aqueous humor.
lens It is a transparent biconvex lens with a diameter of about 9 mm. The lens is located behind the iris. Between the lens at the back and the iris at the front is posterior chamber of the eye containing clear liquid aqueous moisture. Behind the lens is vitreous body. The lens substance is colorless, transparent, dense. The lens has no blood vessels or nerves. The lens is covered with a transparent capsule, which is connected to the ciliary body with the help of the ciliary band. With contraction or relaxation of the ciliary muscle, the tension of the girdle fibers weakens or increases, which leads to a change in the curvature of the lens and its refractive power.
vitreous body fills the entire cavity of the eyeball between the retina at the back and the lens at the front. It consists of a transparent gel-like substance and has no blood vessels.
aqueous humor secreted by the blood vessels of the ciliary processes and the back of the iris. It fills the cavities of the posterior and anterior chambers of the eye, which communicate through the opening of the pupil. Aqueous moisture flows from the posterior chamber to the anterior chamber, and from the anterior chamber to the veins at the border of the cornea and the white of the eye.
1. What structures are part of the organ of vision?
Similar information.
What is called an eye!
The word "eye" even in colloquial speech has different meanings. When they say "he has a thorn in his eye," they mean the eyeball. But if they say "an eye for an eye is needed here", then they obviously mean the intense attention of the entire visual system. Here the eye is identified with vision. In most cases, we will give the word "eye" just such an extended meaning. The eye is the organ of sight, and sometimes just sight. You can say “functions of vision”, or you can say “functions of the eye”.
So, the organ of vision consists of two eyeballs, two optic nerves and a part of the brain that perceives and processes signals transmitted through nerve fibers. As a result, the observed picture is projected back into the space of objects, more or less exactly coinciding with them. The eyeballs are located in the recesses of the skull eye sockets and are driven by muscles.
Eyeball
human eyeball(Fig. 1)

Rice. 1. Horizontal section of the right eyeball: 1 - iris, 2 - lens; 3-axis fixation; 4 - aqueous humor; 5 - cornea; 6 - ciliary muscle; 7-vitreous body; 8 - sclera; 9 - choroid; 10 - retina; 11 - fovea (central fossa); 12-optical axis; 13 - blind spot; 14 - optic nerve (to the brain)
has a shape close to spherical. The outer dense connective tissue membrane of the eyeball, which provides its shape, is called sclera. Its thickness is about 1 mm. Under the sclera there is a more racey - about 0.3 mm - choroid, consisting of a network of blood vessels that feed the eyeball. The inner shell is called the retina or retina. She performs the main function of the eye a: converts light irritation into nervous excitation, performs primary signal processing and sends it to the brain. The fibers of the inner part of the retina pass into the optic nerve, the place of entry of which into the eyeball is called the optic papilla or blind spot.
In the anterior part of the sclera becomes more convex, transparent cornea, or cornea, which is about 0.5 mm thick. The choroid thickens in front and passes into the ciliary body and the iris, in the center of which there is a hole - the pupil. The circular and radial muscle fibers located in the iris produce a constriction or dilation of the pupil. A transparent biconvex lens is attached to the ciliary body - lens.
The space between the cornea and the iris is called front camera the space between the iris and the lens posterior chamber of the eye. Both chambers are filled with a liquid called aqueous humor. The rest of the eyeball cavity between the lens and the retina is filled with a gelatinous substance called the vitreous body.
Nerve connections of the eye
optic nerve 1 (Fig. 2)

Rice. 2. Linking the eye to the brain
consists of nerve fibers - there are about a million of them. On the way to the brain, two nerves cross. The optic chiasm is called the chiasm. After chiasm 2, the optic fibers go further, forming visual canticles 3, and enter parts of the brain called the outer 4 and inner 5 geniculate bodies and the optic tubercle cushion 6. These are intermediate visual centers, the most important of which is the external geniculate body. It consists of six layers in which the fibers of the optic nerve end. From the intermediate centers, excitation is transmitted to the final visual centers in the cortex big brain along the so-called Graziole fibers.
In addition to this direct transmission of excitation from the retinas to the brain centers, there is a complex feedback to control, for example, the movements of the eyeballs. On fig. 2, in the form of a hint of feedback, the initial segments of the 7 oculomotor nerves are shown.
The redistribution of nerve fibers in the chiasm is illustrated in Figure 3.

Rice. 3. Scheme of the course of the optic nerve fibers: 1 - field of view; 2-cornea; 3 - retina; 4 - chiasma; 5 - subcortical visual centers; 6 - Graziola fibers; 7-visual area of the cortex
For each eye (eyeball) can be distinguished temporal and nasal parts of the visual field. The temporal part of one eye is blind, the other eye is on the right, while the left and right parts of the visual field of both eyes are oriented in the same way relative to the eyes. The figure shows only the fibers that transmit the excitation caused by the right side of the visual field. It can be seen that they go to the left half of the brain without crossing each other in the chiasm. If we draw in the same way the fibers representing the left side of the visual field, then it turns out that the fibers of the left eye intersect the fibers representing the right side of the visual field of the right eye. Using a different terminology, we can say that the fibers of the nasal parts of the visual field do not intersect in the chiasm, and the temporal parts do.
Such a course of optic fibers is confirmed by the repeatedly observed cases of hemiopsy - loss of half of the visual field - with damage to one half of the brain. If, for example, the right half of the brain is affected, the person does not see what is to the left of him, but he sees well everything that is located to the right.
On the left side of Fig. Figure 3 shows the sections A, B, C, ... of the visual pathways, and on the right are the schemes for filling these sections with fibers coming from the two halves of the retinas of the left (left column) and right (right column) eyes. Hatching schematically depicts the connection of the fibers passing through the section with the retinas of the eyes. For example, fibers from both halves of the retina of the left eye pass through section A, and the retina of the other eye is not represented at all. Section B shows the temporal parts of both eyes. Sections E, F, G cut only part of the fibers.
It must be said that the path of fibers coming from the central part of the retina is more complex and has not yet been sufficiently studied. More harder way visual stimulation in the brain. In essence, visual impressions and even just "light - the level of external illumination or brightness - affect the human nervous system. Emphasizing the close connection of the eye with the nervous system, the retina is often called the part of the brain that is placed on the periphery.
Oculomotor system
The endings of three pairs of oculomotor muscles are attached to the eyeball, the other ends of which are fastened to various parts of the orbit. It is remarkable that one of the muscles - the upper oblique - is thrown over the block, along which it slides during contraction or relaxation.
The center of rotation of the eyeball lies at a distance of approximately 13.5 mm from the top of the cornea, being very close to the center of the eyeball itself. The mechanism of eye rotation is extremely complex and precise. After all, normally, the axes of both eyes are directed in a coordinated manner to one point - the point of fixation, that is, to the place where the person is looking.
Interaction of parts of the organ of vision
The task of the pupil and transparent media of the eyeball from the cornea to the vitreous - build an image of external objects on the retina. The task of the retina- perceive the image, carry out its primary processing, process light energy into the energy of nerve impulses and send them to the brain along the fibers of the optic nerve. The optic nerve carries impulses to the central nervous system, where they are processed. The information transmitted from the retinas of both eyes is brought together, and a single color three-dimensional image is produced, which our consciousness projects back into the outside world: after all, we perceive the visual image not inside ourselves, but outside, we directly feel objects there (or approximately where they are) are.
The perceived picture is analyzed in various parts of the brain that are no longer related to vision, and as a result of the analysis, decisions are made that often significantly affect human behavior. In addition, in the order of feedback, orders are given to the eyeballs, which turn towards one or another object, and automatic adjustment occurs that does not require control by the human mind: pupil diameter may change, accommodation voltage changes, etc..